Long COVID-19 Symptoms in People with Dementia or Mild Cognitive Impairment
Abstract
What is the impact of long COVID-19 on people with mild cognitive impairment (MCI) or dementia? Self-reported questionnaire was used for the report of long COVID-19 symptoms. People with MCI or dementia or their caregivers regarding patients’ health were recruited COVID-19 throughout from the Athens Alzheimer’s Association. We included 72 participants. Thirty had the diagnosis of MCI and 39 had dementia. Most symptoms lasted for 3-4 weeks. The majority of patients reported having all the symptoms, with fatigue being the major disturbance. The diagnosis and the management of long COVID-19 symptoms requires a more holistic and comprehensive approach.
INTRODUCTION
Even while the COVID-19 pandemic’s effects are less severe now than they were when it first broke out three years ago, they are still felt, particularly by those who are highly vulnerable, with new viral varieties continually proliferating. In a 1-year follow-up study of older adults who were discharged from COVID-19 hospitals, the incidence of cognitive impairment was higher, especially in those with severe cases, than uninfected participants [1]. Further, a systematic review and meta-analysis showed significant neuropsychiatric symptoms in patients with dementia or mild cognitive impairment (MCI) as significant effects of the COVID-19 lockdown [2]. In a large sample 2-year retrospective cohort, the effect of SARS-Cov-2 infection differed by the variants of the virus, with multiple neurological and psychiatric risks (i.e., cognitive deficit, dementia, mood disorder) taking place in the affected population [3].
Regarding long COVID-19, the U.S. Department of Health and Human Services, based on the National Research Action Plan on long COVID-19 and the Services and Supports for Longer-Term Impacts of COVID-19, provided an interim federal working definition. Based on this definition, long COVID-19 is broadly defined as signs, symptoms, and conditions that continue or develop after initial COVID-19 or SARS-CoV-2 infection. The signs, symptoms, and conditions are present four weeks or more after the initial phase of infection; may be multisystemic; and may present with a relapsing–remitting pattern and progression or worsening over time, with the possibility of severe and life-threatening events even months or years after infection. Long COVID-19 is not one condition. It represents many potentially overlapping entities, likely with different biological causes and different sets of risk factors and outcomes. (https://www.covid.gov/longcovid/definitions). Thus, the long-term effect of COVID-19 infection rises broadly, yet remaining unclear how strong it is in already vulnerable groups, such as people with neurodegeneration.
The link between long COVID-19 and dementia is still elusive (https://www.alzforum.org/), with a year after acute illness, some people reporting poor memory and executive function, and Apolipoprotein E ɛ4 carriers being prone to neurovascular complications of COVID-19. More specifically, mild or severe symptoms of COVID-19 seem to worsen existing neurological problems and are associated with decline in speed of processing [1, 2]. A different study showed similar results, with people affected by COVID-19 being at higher risk of developing neurologic conditions, memory problems, strokes, neuropathy, mental health disorders, migraines, or seizures, in the year following the infection [4]. Regarding people with pre-existing dementia, COVID-19 infection can result in the rapid progression of dementia, additional further impairments/deterioration of cognitive abilities, increased fatigue, and increased or new appearance of white matter lesion burden [5]. Existing literature mostly reports the long-term effect of the infection in the general population or the immediate effect of the infection in people with neurodegeneration. What is, however, the long-term effect of COVID-19 infection in people with MCI or dementia?
In an earlier investigation of our team, we showed a significant overall decline of people with MCI or dementia, and more specifically, a big effect on the domains of communication, mood, movement, and compliance with the new measures due to COVID-19 [6]. The prolonged lockdown due to the pandemic resulted in significant further mood and communication decline, in both people with dementia and their caregivers who reported increased physical and psychological burden than before the lockdown period [7]. In the current descriptive work, we took a step further and examined the effect of long-term COVID-19 symptoms in people with MCI or dementia.
METHODS
Our data were collected at the Day-Care Centers of the Athens Alzheimer’s Association. We provided a self-reported questionnaire to functional people with MCI or dementia or to their caregivers, regarding the patient only (no information about the caregivers’ health was collected). Questions referred to the duration of COVID-19 symptoms (3-4 weeks, 2 months, more than 2 months), the type of symptoms (breathing difficulty, fatigue, sore throat, psychological stress/depression), and the effect on the daily living of the person (none, a little bit, considerable, a lot) (see the Supplementary Material). The study took place during the months of September to November 2022. All participants were surveyed at least one month after infection. Lastly, in order to better understand the magnitude of long COVID-19, we included information about the functionality of the patients 1.5 year (mean) before the infection. For these objectives, we used the information from the Instrumental Activities of Daily Living (IADL) questionnaire. Information about their medication and comorbidities was also collected.
The questionnaire was administered in Greek. All participants signed an informed consent regarding the study. The proposal was accepted by the Institutional Review Board of the Athens Alzheimer’s Association. The diagnosis of the cognitive status of each participant was based on an extensive clinical/neurological and neuropsychological evaluation.
Statistical analysis
For the descriptive analysis, we used the Statistical Package for the Social Sciences (SPSS) 28 (SPSS, Chicago, Illinois). Characteristics of people with dementia and their caregivers were analyzed with descriptive statistics (mean, standard deviation, frequency, and percent). On further analysis, we investigated the effects of COVID-19 in the two diagnostic groups (MCI, dementia) separately.
RESULTS
Our sample consisted of 72 participants. Thirty (41.7%) had the diagnosis of MCI, while 39 were people with dementia. They were mostly women (76.4%), with a mean age of 75 years old, and 12 mean years of education (see Table 1). Prior to infection, IADL score was 5.0 (Mean) with SD: 2.76. Regarding the medication of the patients, 22 were taking memantine, 15 antipsychotics, 26 cholinesterase inhibitors, 32 antidepressants, 5 benzodiazepines, 13 neuroleptics, 5 levo-dopa, and 5 dopamine inhibitors. Among the most common comorbidities were the following: hypertension (N = 22), depression (N = 15), and diabetes (N = 10).
Table 1
Characteristics of our sample
| Characteristics | N (%) |
| Diagnosis | |
| MCI | 33 (45.8) |
| Dementia | 39 (54.2) |
| Age, M (SD) | 75.5 (9.3) |
| Sex, women | 55 (76.4) |
| Education, M (SD) | 12.8 (12) |
| Duration of symptoms | |
| 3-4 weeks | 49 (68.1) |
| 2 months | 8 (11.1) |
| >2 months | 15 (20.8) |
| Total | 72 |
Most of the people (68.1%) reported symptoms of long COVID-19 for 3-4 weeks and 11.1% reported symptoms for two months, while a significant 20.8% reported symptoms for more than two months. Strong reference was for all the symptoms (breathing problems, fatigue, sore throat, and psychological distress/depression), with the majority of the patients (62.5%) reporting fatigue as the major disturbance (see Table 1, Fig. 2). This was followed by problems in breathing (61.1%), and psychological distress/depression, affecting 41.7% of the people with MCI or dementia in the study. The symptoms affected patients strongly, with 45.8% reporting “Considerable” disturbance (see Fig. 1).
Fig. 1
Effect of the symptoms on participants.
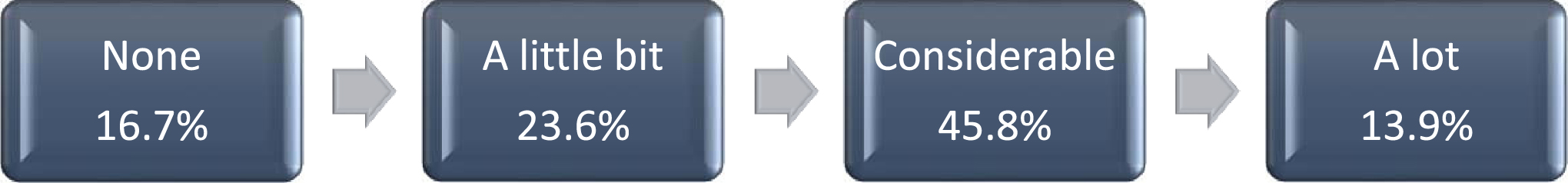
Fig. 2
Symptoms of long COVID-19.
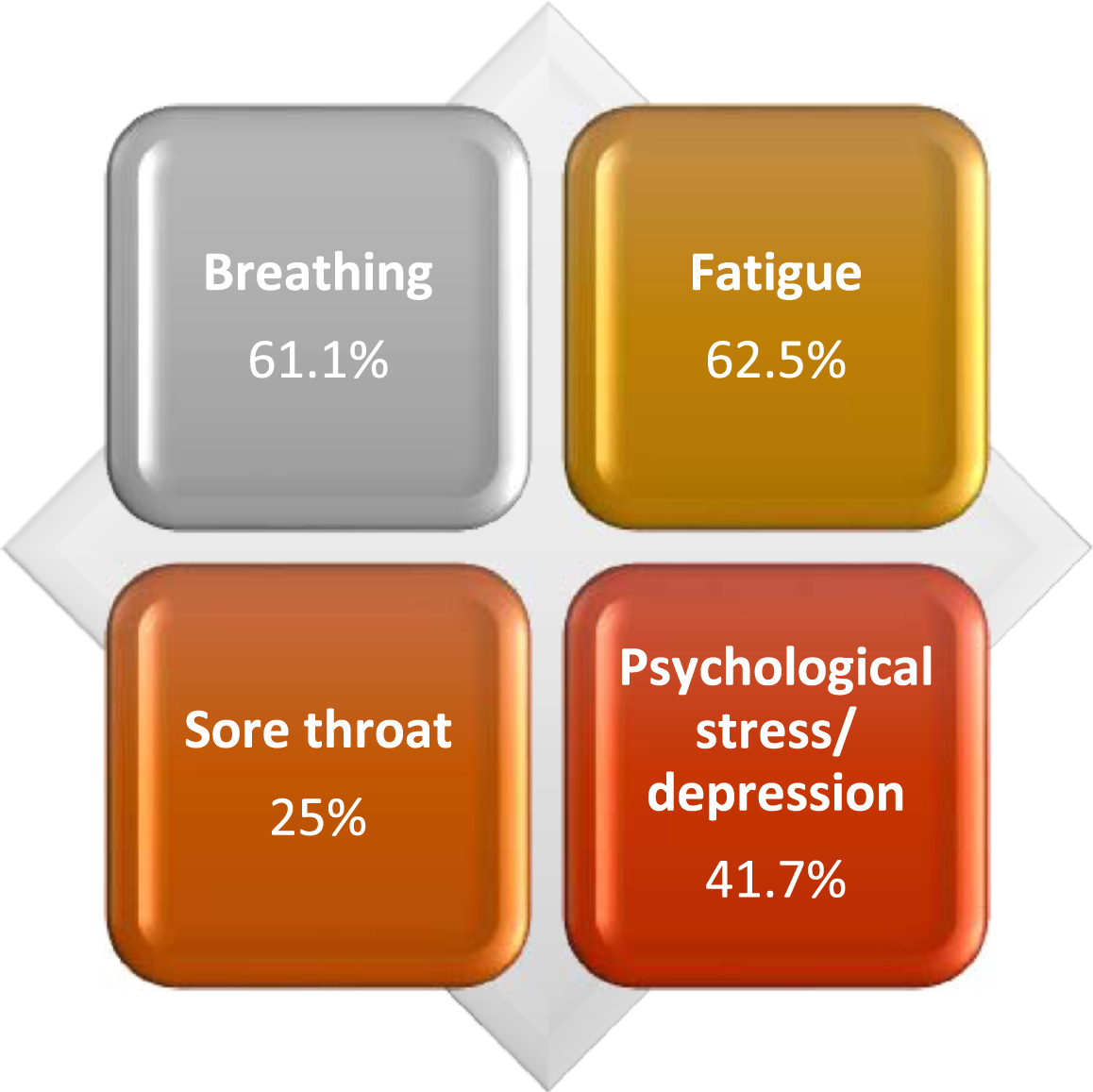
On further analysis based on the clinical diagnosis [MCI (n = 33), dementia (n = 39)], we found the following: most of the MCI participants (72.7%) had long COVID-19 symptoms for 3-4 weeks, while 24.2% had symptoms for more than two months. Regarding the dementia patients, symptoms were reported for 3-4 weeks (64.1%), two months (17.9%), or more than two months (17.9%). The most common long COVID-19 symptom for both MCI and dementia participants was fatigue (63.6% and 61.5%, respectively).
DISCUSSION
Long COVID-19 infection in people with MCI or dementia, besides physical effects such as difficulty in breathing and sore throat, is also linked to increased fatigue and psychological stress/depression. People who are already vulnerable and quite fragile, become even more sensitive to physical and psychological distress. More precisely, we found that the majority of the total sample with MCI or demented with long COVID-19 reported their symptoms to last about 3-4 weeks; with fatigue being the main symptom, considerably affecting them. Interestingly, further analysis by cognitive status showed that the major long COVID-19 symptom for both MCI and demented patients was fatigue.
These striking findings are in accordance with the scarce existing literature, where, in people 65 years or older who were diagnosed with the virus, 32% reported long COVID-19 symptoms, up to four months after the infection [8]. Major symptoms included: respiratory failure, dementia, and fatigue, while these results highlight an excess risk for persistent and new sequelae in older adults. However, the sample of that study included older adults from the general population, and it was not focused on people with MCI or/and dementia.
Longer-term consequences of the infection seem to be likely linked to incident dementia, since longitudinal investigation in non-demented participants has shown that specific brain functions of regions such as the parahippocampal gyrus/perirhinal cortex, and the hippocampus alter after the infection [9]. Regarding people with pre-existing dementia, an increase in symptoms of fatigue and depression seem to follow infection from COVID-19 [5]. However, less is known regarding long COVID-19 situation. Based on a meta-analysis examining the high frequency of cognitive impairment after COVID-19 infection, thirteen studies showed a pattern of cognitive impairment in specific cognitive domains [10]. However, it was not possible to differentiate whether the cognitive impairment found was due to MCI or dementia. Cognitive complaints seem to be frequent in patients with COVID-19, even after the acute phase of the disease [11]. However, the sample of this study included generally-described people with neurological symptoms.
To our knowledge, this is the largest study reporting long COVID-19 symptoms specifically in people with MCI or dementia so far. However, there are some limitations that should be noted; the still relatively small sample size is the main limitation. Further, we used a self-questionnaire instead of any objective method, and lastly, a longitudinal design would benefit the research more.
Long COVID-19 is reported to be similar to other geriatric syndromes, such that the exact mechanism that leads to the symptoms is complex and not clearly understood [8]. Since the most common symptoms of the disease include cough, tiredness, and fever (https://www.who.int/health-topics/coronavirus#tab=tab_3), finding breathing difficulties, fatigue, and sore throat as the most-reported long COVID-19 symptoms does not come as a surprise. The isolation due to the prolonged lockdown might highlight pre-existing neurological or psychiatric symptoms, with the upcoming or current neurodegeneration becoming a booster to these symptoms. Therefore, the diagnosis and the management of long COVID-19 symptoms require a more holistic and comprehensive approach.
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
FUNDING
The authors have no funding to report.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
DATA AVAILABILITY
Data available upon request to the corresponding author.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/ADR-230119.
REFERENCES
[1] | Liu Y-H , Chen Y , Wang Q-H , Wang L-R , Jiang L , Yang Y , Chen X , Li Y , Cen Y , Xu C , Zhu J , Li W , Wang Y-R , Zhang L-L , Liu J , Xu Z-Q , Wang Y-J One-year trajectory of cognitive changes in older survivors of COVID-19 in Wuhan, China: A longitudinal cohort study. JAMA Neurol ((2022) ) 79: , 509–517. |
[2] | Soysal P , Smith L , Trott M , Alexopoulos P , Barbagallo M , Tan SG , Koyanagi A , Shenkin S , Veronese N ; European Society of Geriatric Medicine Special Interest Group in Dementia and Systematic Reviews and Meta-Analyses The effects of COVID-19 lockdown on neuropsychiatric symptoms in patients with dementia or mild cognitive impairment: A systematic review and meta-analysis. Psychogeriatrics ((2022) ) 22: , 402–412. |
[3] | Taquet M , Sillett R , Zhu L , Mendel J , Camplisson I , Dercon Q , Harrison PJ Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: An analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry ((2022) ) 9: , 815–827. |
[4] | Xu E , Xie Y , Al-Aly Z Long-term neurologic outcomes of COVID-19. Nat Med ((2022) ) 28: , 2406–2415. |
[5] | Dubey S , Das S , Ghosh R , Dubey MJ , Chakraborty AP , Roy D , Das G , Dutta A , Santra A , Sengupta S , Benito-León J The effects of SARS-CoV-2 infection on the cognitive functioning of patients with pre-existing dementia. J Alzheimers Dis Rep ((2023) ) 7: , 119–128. |
[6] | Tsapanou A , Papatriantafyllou JD , Yiannopoulou K , Sali D , Kalligerou F , Ntanasi E , Zoi P , Margioti E , Kamtsadeli V , Hatzopoulou M , Koustimpi M , Zagka A , Papageorgiou SG , Sakka P The impact of COVID-19 pandemic on people with mild cognitive impairment/dementia and on their caregivers. Int J Geriatr Psychiatry ((2021) ) 36: , 583–587. |
[7] | Tsapanou A , Zoi P , Kalligerou F , Blekou P , Sakka P The effect of prolonged lockdown due to COVID-19 on Greek demented patients of different stages and on their caregivers. J Alzheimers Dis ((2021) ) 83: , 907–913. |
[8] | Cohen K , Ren S , Heath K , Dasmariñas MC , Jubilo KG , Guo Y , Lipsitch M , Daugherty SE Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: Retrospective cohort study. BMJ ((2022) ) 376: , e068414. |
[9] | Douaud G , Lee S , Alfaro-Almagro F , Arthofer C , Wang C , McCarthy P , Lange F , Andersson JLR , Griffanti L , Duff E , Jbabdi S , Taschler B , Keating P , Winkler AM , Collins R , Matthews PM , Allen N , Miller KL , Nichols TE , Smith SM SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature ((2022) ) 604: , 697–707. |
[10] | Tavares-Junior JWL , de Souza ACC , Borges JWP , Oliveira DN , Siqueira-Neto JI , Sobreira-Neto MA , Braga-Neto P COVID-19 associated cognitive impairment: A systematic review. Cortex ((2022) ) 152: , 77–97. |
[11] | Tavares-Junior JWL , Oliveira DN , da Silva JBS , Feitosa WLQ , Sousa AVM , Cunha LCV , Gaspar SB , Gomes CMP , de Oliveira LLB , Moreira-Nunes CA , Montenegro RC , Sobreira-Neto MA , Braga-Neto P Long-covid cognitive impairment: Cognitive assessment and apolipoprotein E (APOE) genotyping correlation in a Brazilian cohort. Front Psychiatry ((2022) ) 13: , 947583. |



