Traditional Chinese Mind-Body Exercise Baduanjin Modulate Gray Matter and Cognitive Function in Older Adults with Mild Cognitive Impairment: A Brain Imaging Study
Abstract
Background:
Previous studies found traditional Chinese mind-body exercise Baduanjin could modulate cognition of community older adults.
Objective:
This study aims to investigate the effect of 6 months of Baduanjin exercise on brain structure and cognitive function in older adults with mild cognitive impairment (MCI).
Methods:
The MCI older adults were randomly assigned into either Baduanjin training, brisk walking training or usual physical activity control group. Magnetic Resonance Imaging (MRI), Montreal Cognitive Assessment (MoCA) and Wechsler Memory Scale-Chinese Revised (WMS-CR) were applied to measure gray matter volume (GMV), global cognitive ability and memory at baseline and end of intervention.
Results:
Compared to usual physical activity, Baduanjin exercise significantly improved MoCA, WMS-CR scores, WMS-MQ, and mental control and comprehension memory subscores of the WMS-CR; significantly increased the GMV in the temporal gyrus, frontal gyrus, parietal gyrus, medial occipital gyrus, cingulate gyrus and angular gyrus after 6 months of intervention. Compared to brisk walking, Baduanjin significantly improved MoCA scores and picture reproduction subscores of memory, and significantly increased the GMV in the right frontal gyrus, precentral gyrus, occipital gyrus. Furthermore, the increased GMV in the right medial temporal gyrus was significantly associated with improvement in the MoCA scores.
Conclusion:
The present study suggested that regular Baduanjin training could have a positive effect in increasing brain gray matter and improving cognitive function in older adults with MCI.
INTRODUCTION
Mild cognitive impairment (MCI) is a transitional stage between normal aging and dementia with the characteristic of a reduction in memory and/or other cognitive domains with no significant decline in the social and functional activities of daily life [1]. This stage can progress to dementia, mostly in the form of Alzheimer’s disease (AD) [2]. Studies have shown that older adults with MCI developed AD at a rate of 10–30%annually, while those without MCI developed dementia at a rate of 1-2%annually [3]. However, previous studies have shown that individuals with MCI could remain stable or even revert to a normal state if appropriate interventions are adopted [4, 5].
The cognitive decline in older adults with MCI can be attributed in part to structural changes in the brain, such as declines in gray matter volume (GMV) [6]. Furthermore, atrophy of gray matter is associated with the development of mild cognitive impairment [7]. Compared to healthy older people, older adults with MCI experience not only significant cognitive decline but also a higher rate of brain volume loss (notably, gray matter volume loss). Numerous studies have demonstrated that MCI-related brain atrophy is significant in the medial temporal and frontal cortex, superior temporal gyrus, hippocampus, and mesial frontoparietal regions [8, 9]. Therefore, assessment of gray matter volume may allow early detection of MCI and be taken as a marker of intervention efficacy.
Emerging evidence demonstrates that physical activity or exercises not only have positive cognitive effects but also improve brain health for older adults. Some findings in the neuroimaging field have provided evidence that regular exercise has a positive effect in attenuating cognitive impairment and gray matter volume atrophy of the elderly with or without cognitive disorders [10, 11]. Recent longitudinal studies and randomized controlled trials of exercise for healthy older adults also found that participation in exercise programs leads to an improvement in cognitive function and a greater brain volume in specific regions, e.g., in the frontal and temporal lobes [12–14] and hippocampus [15]. Meanwhile, an increasing number of studies have reported positive effects of traditional Chinese mind-body exercises on cognitive ability in different populations [16–18]. However, the mechanisms underlying these improvements remain largely unknown. Many studies assessed structural or functional brain changes regulated by these mind-body exercises using magnetic resonance imaging (MRI), and found that the improvements of cognitive ability were associated with modulating brain structure, brain neural activity, and functional connectivity [19]. As one of traditional Chinese mind-body exercises, Baduanjin exercise only consists of eight separate, delicate and smooth movements with a low-moderate intensity, and is easier to learn than other Chinese mind-body exercises [20]. Baduanjin exercise also a mind-body exercise based on traditional Chinese medicine theories; it emphasizes a combination of symmetrical physical postures, meditative mind and breathing techniques in a harmonious manner and is one of the most common forms of Qigong that has been practiced in China for more than 1000 years [21]. The fundamental assumption is that individuals can regulate thoughts, breathing and body activities by their own internal ability, resulting in enhancement in physical and mental health [22]. Our previous study showed that Baduanjin exercise could significantly increase gray matter volume in the insula, medial temporal lobe, and putamen in healthy older adults [23]. However, it is unclear which specific brain regions are associated with Baduanjin exercise in older adults with MCI. Therefore, we hypothesized that 24 weeks of Baduanjin exercise would decrease brain atrophy progression and improve cognitive impairment in MCI subjects. Here, we report the results of a 24-week randomized controlled trial that suggests that Baduanjin exercise produces positive effects on structural plasticity and cognitive function in older adults with MCI.
MATERIALS AND METHODS
We conducted a 24-week, single-blinded, randomized trial of Baduanjin exercise (ChiCTR-ICR-15005795) at the community centers of Fuzhou city beginning in May 2015 and ending in October 2017. Ethics approval was obtained from the Medical Ethics Committee of the Second People’s Hospital of Fujian Province (No. 2014-KL045-02). Eligible participants were randomly allocated to the Baduanjin exercise (BDJ) group, brisk walking (BWK) group or usual physical activity control (UPA) group. All assessors and data statisticians were blinded to the group allocation of the participants. More detailed information has been reported in our previous published protocol [24].
Participants
Community-dwelling older adults with MCI were recruited from three community centers (Wufeng, Cangxia and Longfeng Community Centers) in Fuzhou, China, by posting posters, sending leaflets and brochures, and setting up a recruiting station at the corresponding community center. Eligibility criteria for inclusion were: (1) aged 60 years or older; (2) suffering from MCI according to Petersen diagnostic criteria [25], including ○1 cognitive decline: MoCA < 26 (if the length of schooling is less than 12 years, then 1 point was added to the examination result),○2 intact activities of daily living (ADL): ADL scores < 18, ○3 absence of dementia (Global deterioration scale, GDS) score at 2 or 3 level; (3) no regular physical exercise for at least half a year (exercise with a frequency of at least twice a week and at least 20 min per session is considered regular exercise); (4) informed consent. Participants were excluded if they reported a history of resistant hypertension, severe visual or hearing loss, severe psychiatric conditions (e.g., severe depression, active suicidal ideation, schizophrenia), alcohol and/or drug abuse. Participants were also excluded if they had current severe medical conditions for which exercise is contraindicated, or had participated in another clinical study.
Intervention
Baduanjin exercise group
The Baduanjin exercise regimen consisted of three 60 min sessions of Baduanjin exercise training per week for a period of 24 weeks. Each session included: 15 minutes warm-up, 40 min Baduanjin training and 5 min cool down. The training scheme was conducted according to the ‘Health Qigong Baduanjin Standard’ published by the State Sports General Administration of China in 2003, and consisted of 8 inherent postures as well as the preparation and ending postures [26]. Professional coaches were employed to guide and supervise their Baduanjin training.
Brisk walking group
The brisk walking workout consisted of three 60 min sessions of brisk walking training per week for a period of 24 weeks. Each session included: 15 min warm-up, 40 min walking and 5 min cool down. Professional coaches were employed to guide participants’ training. The intensity of the exercise was controlled by monitoring participants’ HR at 55–75%of their HR reserve through the Polar heart rate monitor (Mio Sport SD).
Usual physical activity control group
Participants in the control group did not receive any specific exercise intervention and were informed to maintain their original lifestyle.
All participants in three groups received the same cognitive-related health education that involved lectures and discussion providing up-to-date information on topics such as nutrition, health care for the elderly and aging cognitive decline, during one 30 min session every 8 weeks. Participants were not advised to seek any other regular exercise. In order to observe the impact of the usual physical activity, we required all participants to record information about their usual daily physical activity at 1, 13 and 24 weeks of the intervention period on a daily activity log.
Outcome assessment
Demographic characteristics
Participants’ demographic characteristics (e.g., age, gender, living arrangements) and history of disease and medication use were collected at baseline by the recruiters using a self-administered questionnaire.
Cognitive function
Cognitive testing comprised a comprehensive testing battery with a special focus on global cognitive function and memory. All measures were assessed at baseline and end of the interventions using the same versions of the neuropsychological tests by the assessors who were blinded to the assignment group.
Global cognitive function was measured by using the Chinese version of the MoCA scale, which has been proven to be a reliable and effective quantitative assessment of cognitive ability and can be used to track changes in cognitive ability over time in a clinical setting [27, 28]. This scale assessed comprehensive cognitive ability comprised of 7 different cognitive domains including visuospatial/executive functions, naming, attention/concentration, language, abstraction, delayed recall, and orientation with a total score of 0–30 (a higher score equals better function). One point was added to the total score for those with 12 or fewer years of education.
Memory was evaluated using the Wechsler Memory Scale-Chinese Revised (WMS-CR) [29]. It was designed as an assessment instrument for memory function as measured by memory quotient (MQ), as well as memory function subscores (mental control, picture recognition, visual reproduction, associative learning, touch, comprehension memory, and digit span).
Statistical analyses
Statistical analysis was performed using SPSS 21.0 (SPSS Inc., Chicago, IL, United States), with a statistical significance of a two-sided p < 0.05. Baseline characteristics among three groups were compared using one-way analysis of variance (ANOVA) or the Kruskal–Wallis H test for continuous variables and Pearson χ2 or Fisher’s exact test for categorical variables. The group differences of the MoCA and WMS-CR scores among three groups were detected using one-way analysis of variance or the Kruskal–Wallis H test. The post hoc comparison based on Bonferroni method between groups at different time points was conducted using multiple comparisons with adjustment for the type I error rate.
MRI data acquisition
Structural MRI scanning was performed at baseline and at the end of the 24-week intervention using a 3 Tesla GE Signa medical system with an 8-channel head coil. A three-dimensional magnetization prepared rapid acquisition T1-weighted gradient echo (MPRAGE) sequence was used with the sagittal plan: TR = Shortest [Automatic]; TE = 30 ms; slices =164; FOV = 240×240 mm2; slice thickness = 1 mm; inversion time = 450 ms; flip angle = 15°; matrix =256×256; voxel size = 0.93×0.93×1 mm3.
Image processing and voxel-based morphometry (VBM) analysis
Image preprocessing and statistical analyses were performed with SPM12 (Wellcome Institute of Neurology, University College London, United Kingdom) running under MATLAB R2013b (MathWorks, Natick, MA, United States) using Voxel-based morphometry (VBM) toolbox. Data processing steps referred to the voxel based gray matter asymmetry analysis method proposed in 2015 by Kurth et al. [30]. First, the artifacts, pathological and structural abnormalities of all images were examined. Second, three-dimensional images were segmented into cerebrospinal fluid, white matter and gray matter. A specific group template was created to reduce variability between participants, then the images was normalized into the standard Montreal Neurological Institute (MNI) space using the template. Finally, the modulated gray matter images were spatially smoothed, and isotropic Gaussian smoothing with half height and width of 8 mm was selected for convolution; then resampling to 3 mm isotropic voxels to match the same voxel size as preprocessed fMRI data. Thus, for each participant, there was a gray matter volume (GMV) map, and the GMV values were extracted from the GMV map.
Initial general linear model analysis was used to analyze the structural differences of GMV between different groups. Gaussian random-field method (GRF) was used to correct for Voxel p < 0.01 and Cluster p < 0.05, and the activated brain area was defined as the activated range greater than 25 Voxel.
Additional partial Pearson correlation analysis adjusting for age and gender factors was applied to explore the relationship between the GMV changes and behavior measurement changes that displayed significant differences in the above analyses.
RESULTS
Baseline characteristics
A total of 69 participants were consented to undergo MRI scanning at baseline. At trial completion, 9 of the 69 MRI participants dropped out because of training time clashing with other commitments, and 60 participants completed a second MRI scan. No adverse events related Baduanjin exercise and brisk walking occurred during the intervention period. The baseline characteristics of the 69 MRI participants are shown in Table 1. There were no significant differences between the three groups in these baseline characteristics including age, gender, education, smoking, alcohol consumption, hypertension, or other medical history among the three groups.
Table 1
Demographics of the study participants
| Characteristics | BDJ (n = 23) | BWK (n = 23) | UPA (n = 23) | F/χ2 value | p value |
| Age | 65.79±4.35 | 64.88±3.30 | 65.86±5.28 | 0.488 | 0.783 |
| Gender (n) | 6/17 | 11/12 | 6/17 | 3.261 | 0.196 |
| Education (Primary school/Junior high school/Senior high school/More than a high school) (n) | 3/8/6/6 | 3/7/12/1 | 4/5/8/6 | 6.900 | 0.330 |
| Smoking(Yes/No) (n) | 22/1 | 20/3 | 22/1 | 1.725 | 0.422 |
| alcohol(Yes/No) (n) | 22/1 | 17/6 | 21/2 | 5.367 | 0.068 |
| Hypertension (Yes/No) (n) | 11/12 | 13/10 | 15/8 | 1.415 | 0.493 |
| Hyperlipidemia (Yes/No) (n) | 16/7 | 19/4 | 18/5 | 1.139 | 0.566 |
| Diabetes (Yes/No) (n) | 21/2 | 22/1 | 21/2 | 0.431 | 0.806 |
| ADL scores | 14.00±0.00 | 14.00±0.0 | 14.00±0.0 | NA | NA |
| Depression (GDS scores) | 6.09±2.98 | 4.57±2.68 | 5.26±2.75 | 1.694 | 0.192 |
| Activity time during intervention period | |||||
| Sedentary time (hours) | 4.70±1.34 | 4.29±1.45 | 4.85±1.39 | 0.904 | 0.411 |
| Low intensity activity (hours) | 3.35±2.04 | 4.24±1.99 | 3.25±1.87 | 3.703 | 0.157 |
| Moderate intensity activity (hours) | 1.45±0.71 | 0.97±0.75 | 0.53±0.53 | 19.854 | < 0.001 |
BDJ: Baduanjin exercise group; BWK: brisk walking group; UPA: usual physical activity control group. GDS: geriatric depression scale. ADL: activities of daily living.
During intervention period, there was no significant difference in sedentary time and low-intensity activity time among the three groups (p > 0.05), but the moderate-intensity activity time in the Baduanjin group and brisk walking group was significantly longer than in the control group (p < 0.001) (Table 1).
Cognitive measurements
The total scores and subscores of the MoCA and WMS-CR are shown in Table 2. There were no significant differences between the three groups at baseline (pre-intervention) except for the subscores of mental control (100-0) in the WMS-CR (p = 0.019). After the 24-week intervention, multiple comparisons ANOVA found that the BDJ group showed significant increases in the MoCA scores (p = 0.005), the WMS-CR total scores (p = 0.008), WMS-MQ (p = 0.011), and mental control (p = 0.016) and comprehension memory (p = 0.008) subscores compared with the UPA group. Compared to the BWK group, the BDJ group showed significant increases in the MoCA total scores (p = 0.036), and the picture reproduction subscores (p = 0.030) of the WMS-CR, while the BWK group showed significant increases in the mental control subscores of the WMS-CR compared to the UPA group (p = 0.018).
Table 2
Comparison of global cognitive function and memory at baseline and 6-months among groups. Mean (SD)
| Memory | time | UPA (n = 20) | BWK (n = 20) | BDJ (n = 20) | P value |
| MoCA | Baseline | 20.83 (3.27) | 21.65 (2.35) | 22.30 (2.40) | 0.186 |
| 6-month | 21.80 (3.65) | 22.45 (2.40) | 24.30 (1.78)a,b | 0.015 | |
| WMS-CR | Baseline | 76.83 (15.65) | 85.43 (15.23) | 84.87 (17.84) | 0.142 |
| 6-month | 87.30 (20.69) | 93.84 (12.65) | 101.2 (13.14)a | 0.029 | |
| WMS-MQ | Baseline | 93.57 (14.84) | 101.74 (13.71) | 100.91 (16.78) | 0.140 |
| 6-month | 103.2 (19.78) | 109.63 (11.65) | 115.6 (11.33)a | 0.037 | |
| Mental control (0–100) | Baseline | 7.30 (3.08) | 9.00 (2.81) | 8.83 (2.41) | 0.119 |
| 6-month | 7.45 (3.43) | 9.58 (2.24)a | 9.60 (2.35)a | 0.023 | |
| Mental control (100-0) | Baseline | 7.17 (3.53) | 9.74 (2.30) | 9.22 (3.28) | 0.019 |
| 6-month | 8.40 (3.90) | 9.74 (1.97) | 9.90 (2.51) | 0.419 | |
| Mental accumulation | Baseline | 9.52 (2.63) | 9.83 (2.96) | 10.65 (2.60) | 0.288 |
| 6-month | 9.95 (2.98) | 10.74 (1.70) | 10.70 (2.23) | 0.703 | |
| picture recall | Baseline | 7.26 (3.12) | 7.83 (2.55) | 8.52 (3.03) | 0.378 |
| 6-month | 8.85 (3.07) | 9.58 (2.43) | 10.1 (2.92) | 0.379 | |
| Picture recognition | Baseline | 8.52 (3.52) | 9.35 (2.79) | 8.96 (2.46) | 0.817 |
| 6-month | 9.90 (3.24) | 9.95 (3.44) | 11.05 (2.24) | 0.498 | |
| Picture reproduction | Baseline | 8.00 (2.68) | 7.78 (2.47) | 8.04 (2.44) | 0.789 |
| 6-month | 9.20 (2.73) | 8.37 (3.06) | 10.50 (2.14)b | 0.036 | |
| Associative learning | Baseline | 6.78 (2.95) | 7.04 (3.16) | 5.96 (3.32) | 0.477 |
| 6-month | 8.55 (3.20) | 9.84 (2.65) | 10.10 (2.58) | 0.120 | |
| Touch | Baseline | 8.26 (1.54) | 8.48 (1.86) | 8.22 (2.19) | 0.659 |
| 6-month | 9.40 (4.07) | 9.26 (2.47) | 10.00 (3.29) | 0.765 | |
| Comprehension memory | Baseline | 7.00 (2.47) | 8.17 (2.23) | 7.87 (2.16) | 0.207 |
| 6-month | 8.05 (2.21) | 8.84 (1.64) | 9.90 (1.68)a | 0.009 | |
| Digit span | Baseline | 6.57 (3.34) | 8.22 (4.00) | 8.52 (3.33) | 0.143 |
| 6-month | 7.45 (3.07) | 7.95 (3.84) | 9.35 (3.47) | 0.208 |
BDJ: Baduanjin exercise group; BWK: brisk walking group; UPA: usual physical activity control group. a P < 0.05 compared to UPA, b p < 0.05 compared to BWK.
VBM analysis results
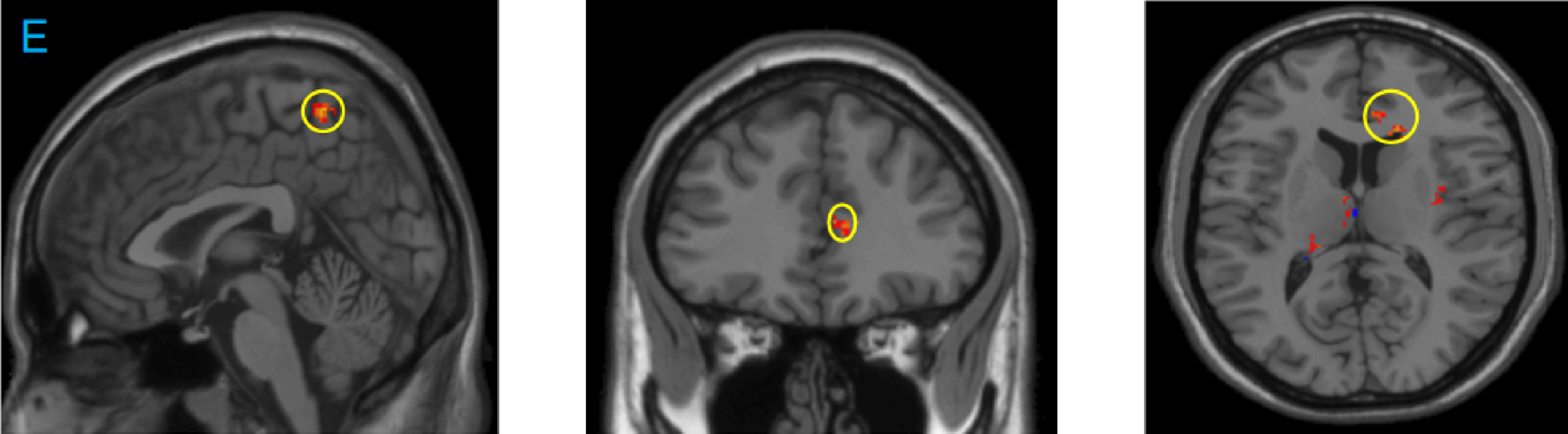
At baseline, there were no significant differences in the GMV of any brain region between the three groups. After 24 weeks of intervention, when compared BDJ group to the UPA group we found significant GMV increases in the temporal gyrus (medial and superior), frontal gyrus (medial and superior), parietal gyrus (superior and inferior), medial occipital gyrus, cingulate gyrus, and angular gyrus; significantly GMV decreases in the postcentral gyrus (Table 3 and Fig. 1). Compared to the BWK group, the following area volumes, including the right frontal gyrus, precentral gyrus, occipital gyrus (superior and medial), were significantly larger in the BDJ group; significantly GMV decreases in the right posterior gyrus, right superior temporal gyrus, occipital gyrus, right precuneus gyrus and left superior frontal gyrus (Table 4 and Fig. 2). Compared to UPA group, the area volumes including the left thalamus, frontal gyrus, right corpus callosum, right anterior cingulate, ventral anterior nucleus, right occipital lobe, left inferior parietal gyrus and precuneus were significantly larger in the BWK group (Table 5 and Fig. 3).
Table 3
Overlap cluster volume between BDJ group and UPA group
| Brain regions | Cluster size | Peak score | MNI peak coordinate (mm) | |||
| x-axis | y-axis | z-axis | ||||
| BDJ > UPA | Left superior temporal gyrus/medial temporal gyrus | 50 | 4.1501 | –60 | –42 | 9 |
| Right superior frontal gyrus/ middle frontal gyrus | 72 | 4.412 | 36 | 54 | 19.5 | |
| Right medial frontal gyrus | 127 | 3.861 | 52.5 | 34.5 | 18 | |
| Right temporal medial gyrus/ occipital medial lobe | 53 | 4.292 | 51 | –67.5 | 28.5 | |
| Left cingulate gyrus | 59 | 3.3676 | –3 | –7.5 | 34.5 | |
| Left superior parietal gyrus | 47 | 3.7661 | –36 | –69 | 49.5 | |
| Right inferior parietal gyrus/angular | 39 | 3.7455 | 46.5 | –67.5 | 48 | |
| UPA > BDJ | Right parietal lobe/posterior central gyrus | 35 | 4.0374 | 57 | –27 | 51 |
BDJ: Baduanjin exercise group; BWK: brisk walking group; UPA: usual physical activity control group.
Fig. 1
Difference of gray matter density between the Baduanjin (BDJ) group and usual physical activity (UPA) control group before and after intervention. A: Brain areas with increased gray matter volume before and after intervention in the BDJ group compared with the UPA group: Left superior temporal gyrus, medial temporal gyrus, right superior frontal gyrus, middle frontal gyrus, right medial frontal gyrus, right temporal medial gyrus, occipital medial lobe, left cingulate gyrus, left superior parietal gyrus, right inferior parietal gyrus, angular; B: right parietal lobe and posterior central gyrus showed decreased gray matter volume in the BDJ group compared with the UPA group.
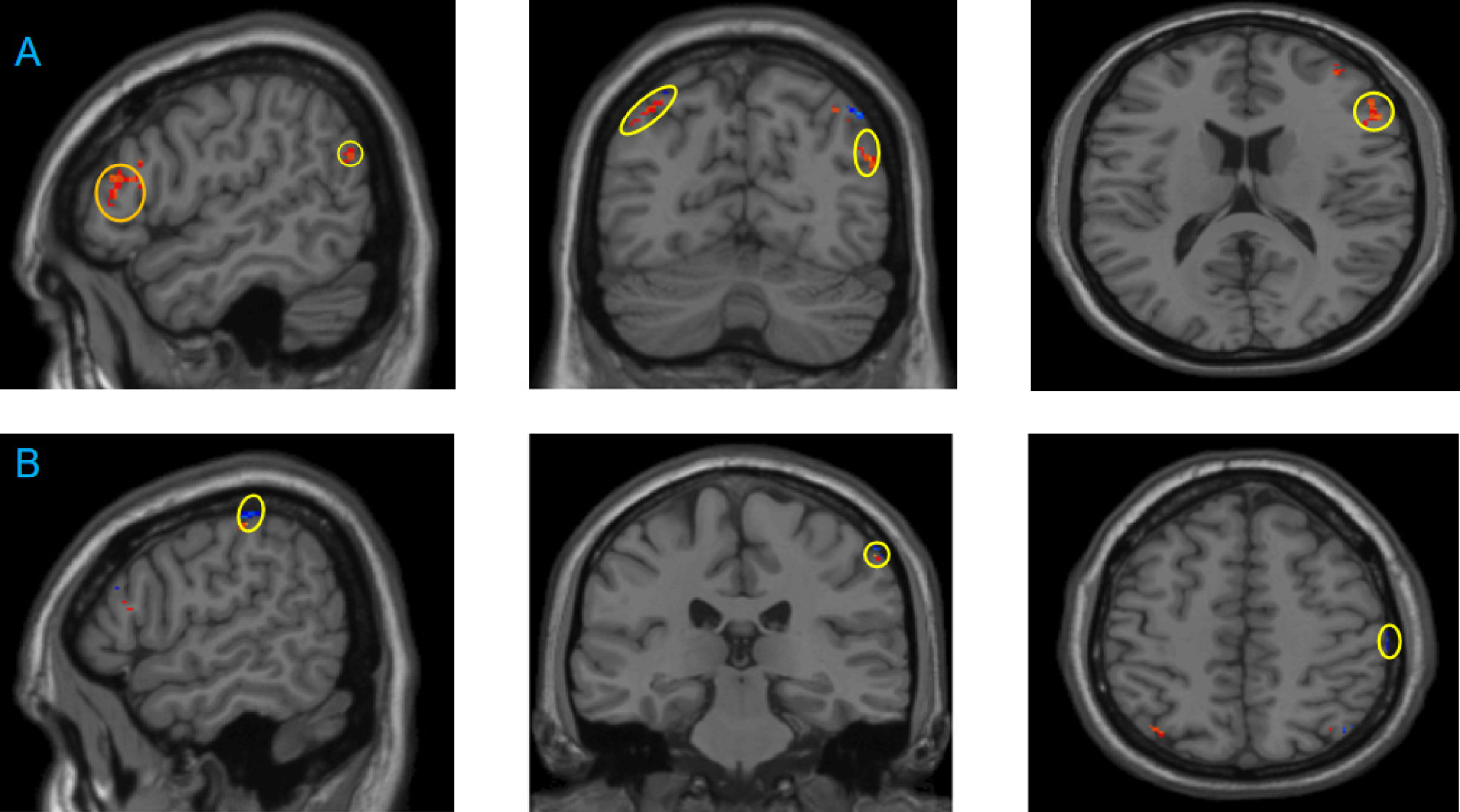
Table 4
Overlap cluster volume between BDJ group and BWK group
| Brain regions | Cluster v | Peak score | MNI peak coordinate (mm) | |||
| x-axis | y-axis | z-axis | ||||
| BDJ > BWK | Right frontal lobe, right precentral gyrus | 37 | 4.8122 | 61.5 | 1.5 | 28.5 |
| Right supraital occipital gyrus, right occipital middle gyrus | 46 | 4.8631 | 33 | –85.5 | 28.5 | |
| Right frontal lobe, | 43 | 3.8707 | 19.5 | –24 | 55.5 | |
| BWK > BDJ | Right cerebellum posterior lobe | 74 | 3.8879 | 3 | –60 | –46.5 |
| Right superior temporal gyrus | 47 | 3.5091 | 40.5 | –46.5 | 13.5 | |
| Right occipital lobe, precuneus | 47 | 4.1311 | 18 | –69 | 18 | |
| Left superior occipital gyrus | 61 | 3.7253 | –37.5 | –90 | 22.5 | |
| Left superior frontal gyrus | 46 | 4.4301 | –19.5 | 12 | 67.5 | |
BDJ: Baduanjin exercise group; BWK: brisk walking group; UPA: usual physical activity control group.
Fig. 2
Difference in gray matter density between the Baduanjin (BDJ) group and the brisk walking (BWK) group before and after the intervention. C: Brain areas with increased gray matter volume in the BDJ group compared with the BWK group: Right frontal lobe, right precentral Gyrus, right supraital Occipital gyrus, right occipital middle gyrus, right frontal lobe; D: compared with the BWK group, there was a decrease in gray matter volume in the BDJ group before and after the intervention: right cerebellar posterior lobe, right superior temporal gyrus, right occipital lobe, right precuneus lobe, left superior occipital gyrus, left superior frontal gyrus.
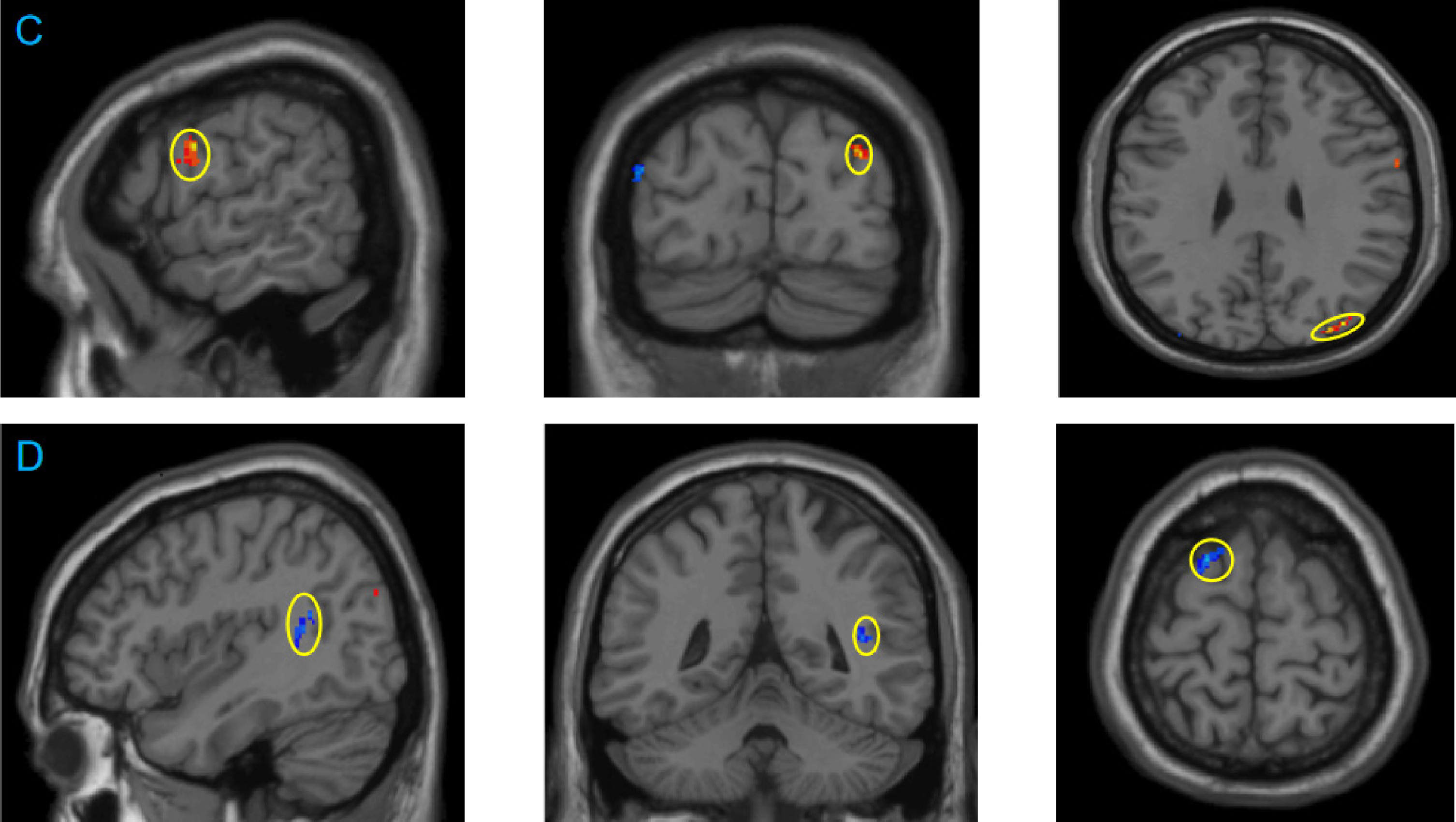
Table 5
Overlap cluster volume between BWKgroup and UPA group
| Brain regions | Cluster size | Peak score | MNI peak coordinate (mm) | |||
| x-axis | y-axis | z-axis | ||||
| BWK > UPA | Left thalamus | 68 | 3.6353 | –6 | –6 | 12 |
| Right frontal lobe | 66 | 4.525 | 39 | –4.5 | 195 | |
| Right corpus callosum | 40 | 4.1164 | 16.5 | 27 | 12 | |
| Right anterior cingulate | 36 | 4.5263 | 6 | 36 | 12 | |
| Left thalamus, ventrolateral nucleus | 151 | 3.7626 | –9 | –7.5 | 18 | |
| Right occipital lobe, precuneus | 45 | 4.1333 | –4.5 | –9 | 33 | |
| Left inferior parietal lobe | 35 | 4.0419 | –37.5 | –58.5 | 45 | |
| right frontal lobe, precuneus | 58 | 4.933 | 1.5 | –48 | 61.5 | |
BDJ: Baduanjin exercise group; BWK: brisk walking group; UPA: usual physical activity control group.
Fig. 3
Difference in gray matter density between the brisk walking (BWK) group and usual activity physical (UPA) control group before and after the intervention. E: Brain areas with increased gray matter volume in the BWK group compared with the UPA group: left thalamus, right frontal lobe, right corpus callosum, right anterior cingulate gyrus, left thalamus, ventrolateral nucleus, right occipital lobe, precuneus, left inferior parietal lobe, right frontal lobe and precuneus.
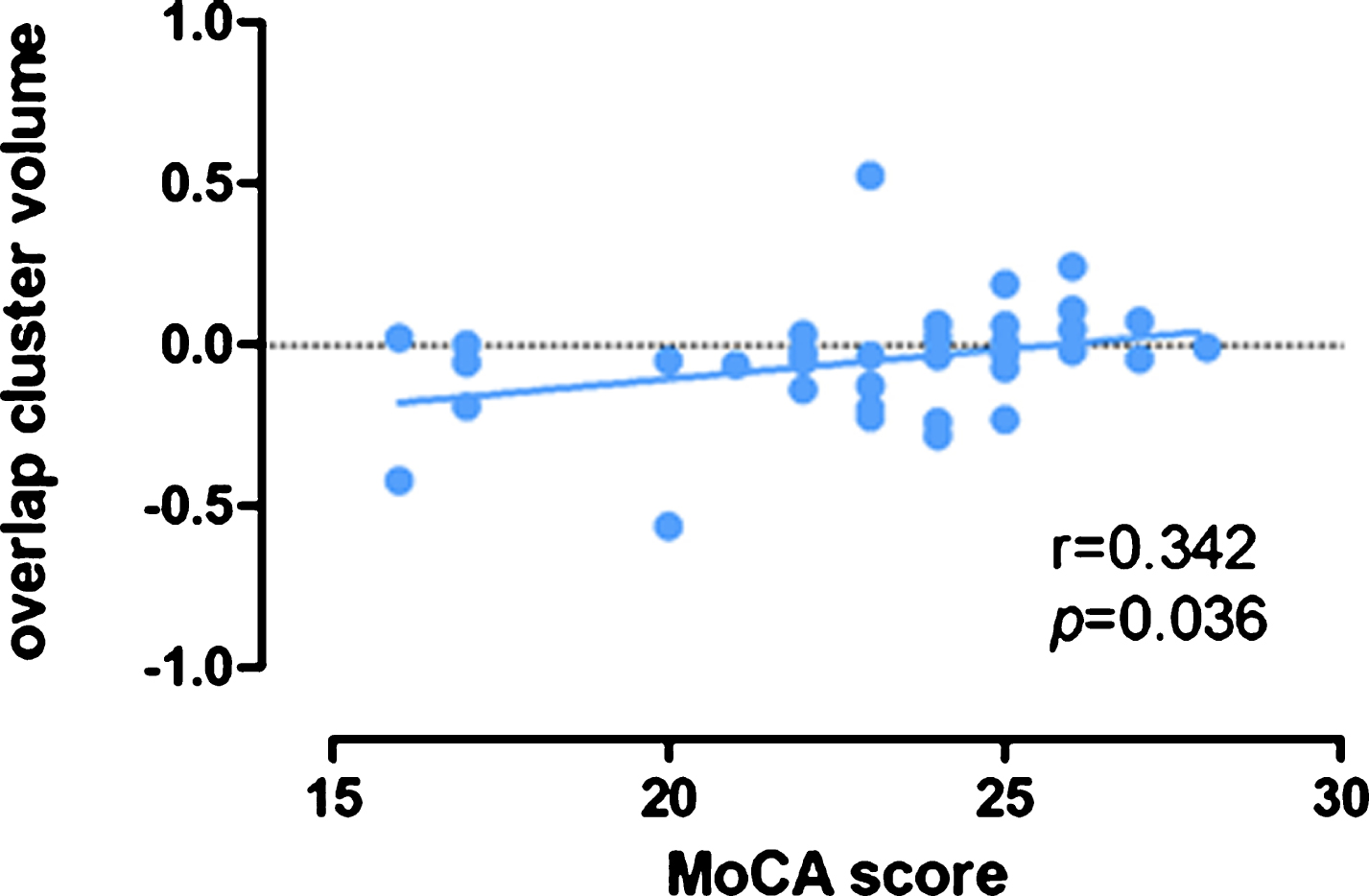
Additional correlation analyses
To investigate the association between the GMV changes and cognitive outcome changes (i.e., only the cognitive outcomes that showed a significant difference among groups). We extracted the average GMV values of the significantly altered clusters (shown in Table 3–5) and performed a partial correlation analysis. After adjusting for age, gender and education factors, the results showed that the increased GMV in the right medial temporal gyrus was significantly associated with improvement in the MoCA total scores (p = 0.036, r = 0.342) (Fig. 4).
Fig. 4
The gray matter density in right middle temporal gyrus were positively correlated with MoCA scores. Scatter plots show the significant associated between GMV increase in right middle temporal gyrus (post-pre) and improvement in MoCA scores (post-pre) adjusted for age, gender and education.
DISCUSSION
The present study aimed to investigate the effect of a 24-week training protocol in Baduanjin, a traditional Chinese mind-body exercise, on global cognitive function, memory and gray matter volume (GMV) of the brain in older adults with MCI. We found that compared with the usual physical activity control group, the Baduanjin exercise group showed significantly increased the GMV in the temporal gyrus, frontal gyrus, parietal gyrus, medial occipital gyrus, cingulate gyrus and angular gyrus; significantly improved MoCA scores, WMS-CR total scores, WMS-MQ, mental control, and comprehension subscores. We also found that the Baduanjin exercise group had improved MoCA scores and WMS-CR scale picture reproduction subscores, and increased GMV in the right frontal gyrus, precentral gyrus and occipital gyrus compared with the BWK group. In addition, this study found that the right medial temporal gyrus was significantly associated with improvement in the MoCA-scores.
Baduanjin exercise is one of most popular traditional Chinese mind-body exercises in China, which may date back to the Song Dynasty (960–1279). In contrast to the conventional aerobic or resistance exercise modalities, Baduanjin exercise has several components, including physical, cognitive and social, and it not only focuses on strengthening physical function but also emphasizes that breathing integrated with body motions achieves a harmonious balance between body and mind, which are believed to aid in maintaining cognition in older adults [31]. Previous studies have suggested beneficial effects of traditional Chinese mind-body exercise on global cognitive function and memory in MCI or healthy older adults [32, 33]. For example, in a hybrid observational study of healthy, nonsedentary adults, a positive association between long-term traditional Chinese mind-body exercise (Tai Chi) and preservation of cognitive function was observed [17]. A recent cross-sectional study also reported that traditional Chinese mind-body exercise (Tai Chi) had a more positive association with cognitive function than did conventional aerobic exercise (brisk walking) in older adults [34]. Our previous studies have also shown that 12 weeks of Baduanjin training improved the WMS-CR scores in older adults compared to the control group [23]. These results are consistent with the present study, indicating that Baduanjin exercise may have a positive benefit in improving global cognitive function and memory among older adults with MCI.
In this study, we found a significant gray matter volume (GMV) increase in the temporal lobe after Baduanjin exercise, moreover, the gray matter volume of right medial temporal lobe was significantly correlated with the MoCA score. As we all known, atrophy of the medial temporal lobe exacerbates brain aging, and it can lead to decreased memory and cognitive function [35], previous study has identified medial temporal lobe atrophy as a clinical marker of progression from mild cognitive impairment to dementia [36], Siddarth and colleagues [37] found the elders with higher physical activity exhibited superior cognitive performance and thicker sub-regions of medial temporal lobe. Our previous research has also found significant GMV increases at the left medial temporal lobe after Baduanjin exercise compared to the control group among healthy older adults [23]. Current results also supported these previous findings and suggested an important role for the medial temporal lobe in the modulatory effect of Baduanjin exercise on the preservation of cognitive function in MCI patients.
Current study showed GMV increase in the frontal gyrus, cingulate gyrus and occipital lobe after Baduanjin and brisk walking exercise compared with the UPA group. Tabei and colleagues [38] demonstrated that compared to the control group, physical exercise induces increased GMV in the frontal lobe. Hashimoto and colleagues [39] confirmed that high intensity aerobic exercise would increase cortical activation of the frontal lobe. There was another study showed that compared to omega-3 fatty acid supplementation and cognitive stimulation, the aerobic exercise combined omega-3 fatty acid supplementation and cognitive stimulation retained or even increased the frontal, cingulate and parietal gray matter volume in MCI patients [40]. The occipital lobe is the visual processing center of the brain and is associated with short-term, visual and working memory [41]. Alexopoulos et al. [42] observed lower perfusion in the left middle occipital lobe in MCI patients. Makizako et al. [43] found that a greater 6 min walking distance performance was positively linked to better memory function and increased GMV in the middle occipital gyrus among MCI patient. Current study showed 24 weeks of Baduanjin and brisk walking training improved the GMV in the frontal gyrus, cingulate gyrus and medial occipital gyrus in MCI older adults. Our findings were consistent with these previous results suggesting a potential role of the frontal gyrus, cingulate gyrus and occipital gyrus in the modulation effect of Baduanjin and brisk walking exercise.
We also found GMV increases in the parietal gyrus and angular gyrus after Baduanjin exercise, and increases in thalamus, ventral anterior nucleus, left inferior parietal gyrus and precuneus after brisk walking training. Studies reported the older adults with MCI compared to healthy control showed a significant decrease in the parietal lobe [44], angular gyrus [45], bilateral thalamus and left precuneus [46], and the atrophy of left precuneus and thalamus were a risk factor of memory. But our study did not find significant positive effects of the 24-week brisk walking intervention on cognitive behavior. We speculate it may be that brisk walking is more focused on the improvement of exercise ability in the elderly, and the improvement of cognitive function may not be obvious. In addition, we also found the significant difference of GMV in frontal lobe, occipital gyrus, precuneus and right cerebellum posterior lobe between Baduanjin and brisk walking group. These findings indicate the mechanisms underlying Baduanjin and brisk walking training may differ. Compared to brisk walking, Baduanjin exercise might have lower exercise intensity and energy expenditure but emphasize more coordination of both body and mind. A recent systematic review on MRI studies has suggested that the exercises with coordination of body and mind could modulate brain structure, mainly in in the prefrontal cortex, hippocampus/medial temporal lobe, lateral temporal lobe, insula, and the cingulate cortex [19].
Several possible limitations should be considered when interpreting our findings. First, the sample size was relatively small. Although enough subjects were recruited in this study, only some of them consented to the MRI scans; therefore, a future study with a larger sample size is needed to further confirm the findings of our study. Second, we designed a conventional aerobic exercise (brisk walking) intervention as the positive control group, as studies have demonstrated the positive effect of aerobic exercise on cognitive function among MCI subjects [24, 47, 48], and the aim was to compare the effect of traditional Chinese mind-body exercise with aerobic exercise on cognitive function among MCI subjects. However, we did not observe significant positive effects of the 24-week brisk walking intervention on most of the measured cognition-related outcomes. The possible causes may come from not quantifying the exercise intensity of the brisk walking program in this study. Therefore, the present study cannot identify whether Baduanjin exercise is superior to a brisk walking intervention in improving cognitive function. Future studies should quantify a participants’ exercise intensity while brisk walking by measuring peak oxygen consumption. Furthermore, because the etiology of MCI in the subjects is not yet know, MCI disease may response differently to different types of exercise. Therefore, the mechanisms by which Baduanjin exercise leads to improved cognition on cellular level should be further explored. In addition, Baduanjin exercise is one of most popular traditional Chinese mind-body exercises in the Chinese population, and it is difficult to blind the participants in the research of exercise intervention; therefore, participants in this group may have had greater subjective expectations than other groups, which may have influenced the results.
CONCLUSIONS
Exposure of MCI older adults to 24 weeks of Baduanjin exercise improved global cognitive function and global memory, as well as improved aspects of memory function. Meanwhile, increased GMV in the temporal gyrus, frontal gyrus, occipital lobe, cingulate gyrus and parietal gyrus was observed. Overall, our results suggest that Baduanjin might be a promising approach to increase gray matter volume and improve cognitive function in MCI older adults.
AUTHOR CONTRIBUTIONS
GHZ conceived and designed the study. BZY and GHZ wrote the manuscript. BZY, RX, PTQ, MYL, YHZ, ZYX managed the training location. All authors contributed to drafting the manuscript and have read and approved the final manuscript.
FUNDING
This study is supported by the National Natural Science Foundation of China (http://www.nsfc.gov.cn, grant no.82074510, 81574045).
ACKNOWLEDGMENTS
We thank the participants and staff at the communities and hospitals for their work in this project, including Fujian University of Traditional Chinese Medicine Subsidiary Rehabilitation Hospital.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
REFERENCES
[1] | Petersen RC . Mild cognitive impairment as a diagnostic entity. J Intern Med. (2004) ;256: (3):183–94. |
[2] | Koyanagi A , Lara E , Stubbs B , Carvalho AF , Oh H , Stickley A , Veronese N , Vancampfort D . Chronic Physical Conditions, Multimorbidity, and Mild Cognitive Impairment in Low- and Middle-Income Countries. J Am Geriatr Soc. (2018) ;66: (4):721–7. |
[3] | Burns A , Zaudig M . Mild cognitive impairment in older people. Lancet. 360. (2002) ;360: (9349):1963–5. |
[4] | Jones JD , Kuhn TP , Szymkowicz SM . Reverters from PD-MCI to cognitively intact are at risk for future cognitive impairment: Analysis of the PPMI cohort. Parkinsonism Relat Disord. (2018) ;47: :3–7. |
[5] | Sachdev PS , Lipnicki DM , Crawford J , Reppermund S , Kochan NA , Trollor JN , Wen W , Draper B , Slavin MJ , Kang K , Lux O , Mather KA , Brodaty H ; Sydney Memory, Ageing Study Team. Factors predicting reversion from mild cognitive impairment to normal cognitive functioning: a population-based study. PLoS One. (2013) ;8: (3):e59649. |
[6] | Lin AL , Laird AR , Fox PT , Gao JH . Multimodal MRI neuroimaging biomarkers for cognitive normal adults, amnestic mild cognitive impairment, and Alzheimer’s disease. Neurol Res Int. (2012) ;2012: :907409. |
[7] | Pini L , Pievani M , Bocchetta M , Altomare D , Bosco P , Cavedo E , Galluzzi S , Marizzoni M , Frisoni GB . Brain atrophy in Alzheimer’s Disease and aging. Ageing Res Rev. (2016) ;30: :25–48. |
[8] | Minkova L , Habich A , Peter J , Kaller CP , Eickhoff SB , Klöppel S . Gray matter asymmetries in aging and neurodegeneration: A review and meta-analysis. Hum Brain Ma. (2017) ;38: (12):5890–904. |
[9] | Sheelakumari R , Kesavadas C , Lekha VS , Justus S , Sarma PS , Menon R . Structural correlates of mild cognitive impairment: A clinicovolumetric study. Neurol India. (2018) ;66: (2):370–6. |
[10] | Li MY , Huang MM , Li SZ , Tao J , Zheng GH , Chen LD . The effects of aerobic exercise on the structure and function of DMN-related brain regions: a systematic review. Int J Neurosci. (2017) ;127: (7):634–49. |
[11] | Song D , Yu DSF , Li PWC , Lei Y . The effectiveness of physical exercise on cognitive and psychological outcomes in individuals with mild cognitive impairment: A systematic review and meta-analysis. Int J Nurs Stud. 2018:155-64. |
[12] | Liu-Ambrose T , Nagamatsu LS , Voss MW , Khan KM , Handy TC . Resistance training and functional plasticity of the aging braa 12-month randomized controlled trial. Neurobiol Aging. (2012) ;33: (8):1690–8. |
[13] | Tamura M , Nemoto K , Kawaguchi A , Kato M , Arai T , Kakuma T , Mizukami K , Matsuda H , Soya H , Asada T . Long-term mild-intensity exercise regimen preserves prefrontal cortical volume against aging. Int J Geriatr Psychiatry. (2015) ;30: (7):686–94. |
[14] | Yuki A , Lee S , Kim H , Kozakai R , Ando F , Shimokata H . Relationship between physical activity and brain atrophy progression. Med Sci Sports Exerc. (2012) ;44: (12):2362–8. |
[15] | ten Brinke LF , Bolandzadeh N , Nagamatsu LS , Hsu CL , Davis JC , Miran-Khan K , Liu-Ambrose T . Aerobic exercise increases hippocampal volume in older women with probable mild cognitive impairment: a 6-month randomised controlled trial. Br J Sports Med. (2015) ;49: (4):248–54. |
[16] | Miller SM , Taylor-Piliae RE . Effects of Tai Chi on cognitive function in community-dwelling older adults: a review. Geriatr Nurs. (2014) ;35: (1):9–19. |
[17] | Walsh JN , Manor B , Hausdorff J , Novak V , Lipsitz L , Gow B , Macklin EA , Peng CK , Wayne PM . Impact of Short- and Long-term Tai Chi Mind-Body Exercise Training on Cognitive Function in Healthy Adults: Results From a Hybrid Observational Study and Randomized Trial. Glob Adv Health Med. (2015) ;4: (4):38–48. |
[18] | Sungkarat S , Boripuntakul S , Kumfu S , Lord SR , Chattipakorn N . Tai Chi Improves Cognition and Plasma BDNF in Older Adults With Mild Cognitive Impairment: A Randomized Controlled Trial. Neurorehabil Neural Repair. (2018) ;32: (2):142–9. |
[19] | Zhang X , Zong B , Zhao W , Li L . Effects of Mind-Body Exercise on Brain Structure and Function: A Systematic Review on MRI Studies. Brain Sci. (2021) ;11: (2):205. |
[20] | Koh TC . Baduanjin –an ancient Chinese exercise. Am J Chin Med. (1982) ;10: (1-4):14–21. |
[21] | Cheng FK . Effects of Baduanjin on mental health: a comprehensive review. J Bodyw Mov Ther. (2015) ;19: (1):138–49. |
[22] | Chan AS , Cheung MC , Tsui WJ , Sze SL , Shi D . Dejian mind-body intervention on depressive mood of community-dwelling adults: a randomized controlled trial. Evid Based Complement Alternat Med. (2011) ;2011: :473961. |
[23] | Tao J , Liu J , Liu W , Huang J , Xue X , Chen X , Wu J , Zheng G , Chen B , Li M , Sun S , Jorgenson K , Lang C , Hu K , Chen S , Chen L , Kong J . Tai Chi Chuan and Baduanjin Increase Grey Matter Volume in Older Adults: A Brain Imaging Study. J Alzheimers Dis. (2017) ;60: (2):389–400. |
[24] | Zheng G , Xia R , Zhou W , Tao J , Chen L . Aerobic exercise ameliorates cognitive function in older adults with mild cognitive impairment: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. (2016) ;50: (23):1443–50. |
[25] | Petersen RC . Mild cognitive impairment as a diagnostic entity. J Intern Med. (2004) ;256: (3):183–94. |
[26] | Health Qigong Management Center of General Administration of Sport of China. Health Qigong-Baduanjin: Beijing: People’s Sports Publishing House of China; (2003) . |
[27] | Koski L , Xie H , Finch L . Measuring cognition in a geriatric outpatient clinic: Rasch analysis of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol. (2009) ;22: (3):151–60. |
[28] | Zhou S , Zhu J , Zhang N , Wang B , Li T , Lv X , Ng TP , Yu X , Wang H . The influence of education on Chinese version of Montreal cognitive assessment in detecting amnesic mild cognitive impairment among older people in a Beijing rural community. ScientificWorldJournal. (2014) ;2014: :689456. |
[29] | Liu L . The application of Wechsler Memory Scale revised in China in Chinese children. Chinese Journal of Clinical Psychology. (2009) ;6: :705–7. |
[30] | Kurth F , Gaser C , Luders E . A 12-step user guide for analyzing voxel-wise gray matter asymmetries in statistical parametric mapping (SPM). Nat Protoc. (2015) ;10: (2):293–304. |
[31] | Zou L , Pan Z , Yeung A , Talwar S , Wang C , Liu Y , Shu Y , Chen X , Thomas GA . A Review Study on the Beneficial Effects of Baduanjin. J Altern Complement Med. (2018) ;24: (4):324–35. |
[32] | Zheng G , Liu F , Li S , Huang M , Tao J , Chen L . Tai Chi and the Protection of Cognitive Ability: A Systematic Review of Prospective Studies in Healthy Adults. Am J Prev Med. (2015) ;49: (1):89–97. |
[33] | Zheng W , Xiang YQ , Ungvari GS , Chiu HFK , Ning YP , Yu X , Forester BP , Xiang YT . Tai chi for mild cognitive impairment: a systematic review. Psychogeriatrics. (2017) ;17: (6):514–6. |
[34] | Ji Z , Li A , Feng T , Liu X , You Y , Meng F , Wang R , Lu J , Zhang C . The benefits of Tai Chi and brisk walking for cognitive function and fitness in older adults. PeerJ. (2017) ;5: :e3943. |
[35] | Ward AM , Mormino EC , Huijbers W , Schultz AP , Hedden T , Sperling RA . Relationships between default-mode network connectivity, medial temporal lobe structure, and age-related memory deficits. Neurobiol Aging. (2015) ;36: (1):265–72. |
[36] | Persson K , Barca ML , Eldholm RS , Cavallin L , Šaltytė Benth J , Selbæk G , et al. Visual Evaluation of Medial Temporal Lobe Atrophy as a Clinical Marker of Conversion from Mild Cognitive Impairment to Dementia and for Predicting Progression in Patients with Mild Cognitive Impairment and Mild Alzheimer’s Disease. Dement Geriatr Cogn Disord. (2017) ;44: (1-2):12–24. |
[37] | Siddarth P , Rahi B , Emerson ND , Burggren AC , Miller KJ , Bookheimer S , et al. Physical Activity and Hippocampal Sub-Region Structure in Older Adults with Memory Complaints. J Alzheimers Dis. (2018) ;61: (3):1089–96. |
[38] | Tabei KI , Satoh M , Ogawa JI , Tokita T , Nakaguchi N , Nakao K , et al. Physical Exercise with Music Reduces Gray and White Matter Loss in the Frontal Cortex of Elderly People: The Mihama-Kiho Scan Project. Front Aging Neurosci. (2017) ;9: :174. |
[39] | Hashimoto N , Yokogawa M , Kojima H , Tanaka S , Nakagawa T . Effect of moderate exercise intensities on the cortical activity in young adults. J Phys Ther Sci. (2018) ;30: (10):1257–61. |
[40] | Köbe T , Witte AV , Schnelle A , Lesemann A , Fabian S , Tesky VA , Pantel J , Flöel A . Combined omega-3 fatty acids, aerobic exercise and cognitive stimulation prevents decline in gray matter volume of the frontal, parietal and cingulate cortex in patients with mild cognitive impairment. Neuroimage. (2016) ;131: :226–38. |
[41] | van Dam WO , Decker SL , Durbin JS , Vendemia JM , Desai RH . Resting state signatures of domain and demand-specific working memory performance. Neuroimage. . (2015) ;118: :174–82. |
[42] | Alexopoulos P , Sorg C , Förschler A , Grimmer T , Skokou M , Wohlschläger A , et al. Perfusion abnormalities in mild cognitive impairment and mild dementia in Alzheimer’s disease measured by pulsed arterial spin labeling MRI. Eur Arch Psychiatry Clin Neurosci. (2012) ;262: (1):69–77. |
[43] | Makizako H , Shimada H , Doi T , Park H , Yoshida D , Suzuki T . Six-minute walking distance correlated with memory and brain volume in older adults with mild cognitive impairment: a voxel-based morphometry study. Dement Geriatr Cogn Dis Extra. (2013) ;3: (1):223–32. |
[44] | Oishi A , Yamasaki T , Tsuru A , Minohara M , Tobimatsu S . Decreased Gray Matter Volume of Right Inferior Parietal Lobule Is Associated With Severity of Mental Disorientation in Patients With Mild Cognitive Impairment. Front Neurol. (2018) ;9: :1086. |
[45] | Griffith HR , Stewart CC , Stoeckel LE , Okonkwo OC , den Hollander JA , Martin RC , et al. Magnetic resonance imaging volume of the angular gyri predicts financial skill deficits in people with amnestic mild cognitive impairment. J Am Geriatr Soc. (2010) ;58: (2):265–74. |
[46] | Qin R , Li M , Luo R , Ye Q , Luo C , Chen H , Qian L , Zhu X , Bai F , Zhang B , Liu R , Zhao H , Xu Y . The efficacy of gray matter atrophy and cognitive assessment in differentiation of aMCI and naMCI. Appl Neuropsychol Adult. (2020) ;16: :1–7. |
[47] | Cammisuli DM , Innocenti A , Franzoni F , Pruneti C . Aerobic exercise effects upon cognition in Mild Cognitive Impairment: A systematic review of randomized controlled trials. Arch Ital Biol. (2017) ;155: (1-2):54–62. |
[48] | Zheng G , Huang M , Li S , Li M , Xia R , Zhou W , Tao J , Chen L . Effect of Baduanjin exercise on cognitive function in older adults with mild cognitive impairment: study protocol for a randomised controlled trial. BMJ Open. (2016) ;6: (4):e010602. |



