Challenging Cases in Urothelial Cancer: Case 27
A 67 year old woman with congestive heart failure underwent an extensive medical evaluation prior to consideration for a heart transplant. She has a 20 year history of cardiomyopathy. In 2015 she developed recurrent ventricular tachycardia and had an implantable cardioverter/defibrillator (ICD) placed and underwent cardiac ablation. In 2020 she had worsening of the CHF and recurrent ventricular tachycardia. A left ventricular assist device (LVAD) was placed. During this procedure a rotary pump is inserted next to the left ventricle. The pump is connected to the left ventricle and the ascending aorta by grafts. The patient’s performance status greatly improved. The LVAD requires the patient to remain on anticoagulation, e.g. warfarin.
The patient had no voiding complaints. Prior to the placement of the LVAD she had not had major surgery. She has never smoked cigarettes.
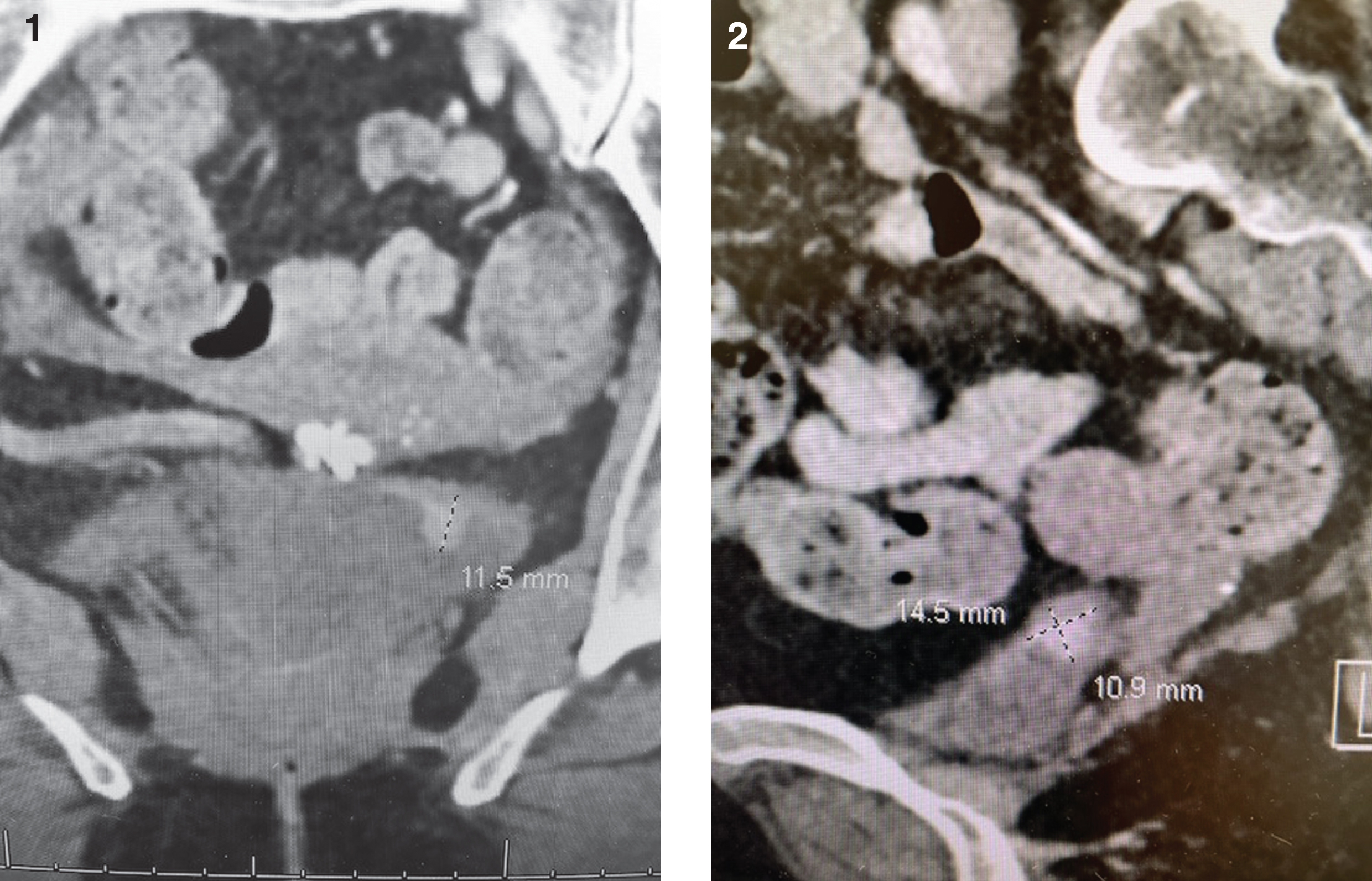
As part of her evaluation for consideration of a heart transplant she had a CT scan of the abdomen and pelvis. The upper urinary tract was normal. The images identified a nodular wall enhancement of the left lateral urinary bladder which measured approximately 1.5×1.0 cm. Figs. 1, 2. The radiologist recommended further evaluation.
Figs. 1-2
Coronal and sagital planes identifying the small bladder tumor.
A flexible cystoscopy confirmed the presence of a papillary tumor on the left lateral/posterior wall. The tumor appeared to be confined to the urothelium.
In preparation for a transurethral resection of the solitary tumor she stopped the warfarin and was placed on a heparin drip, transitioned to a low molecular weight heparin bridge, and postoperatively resumed warfarin.
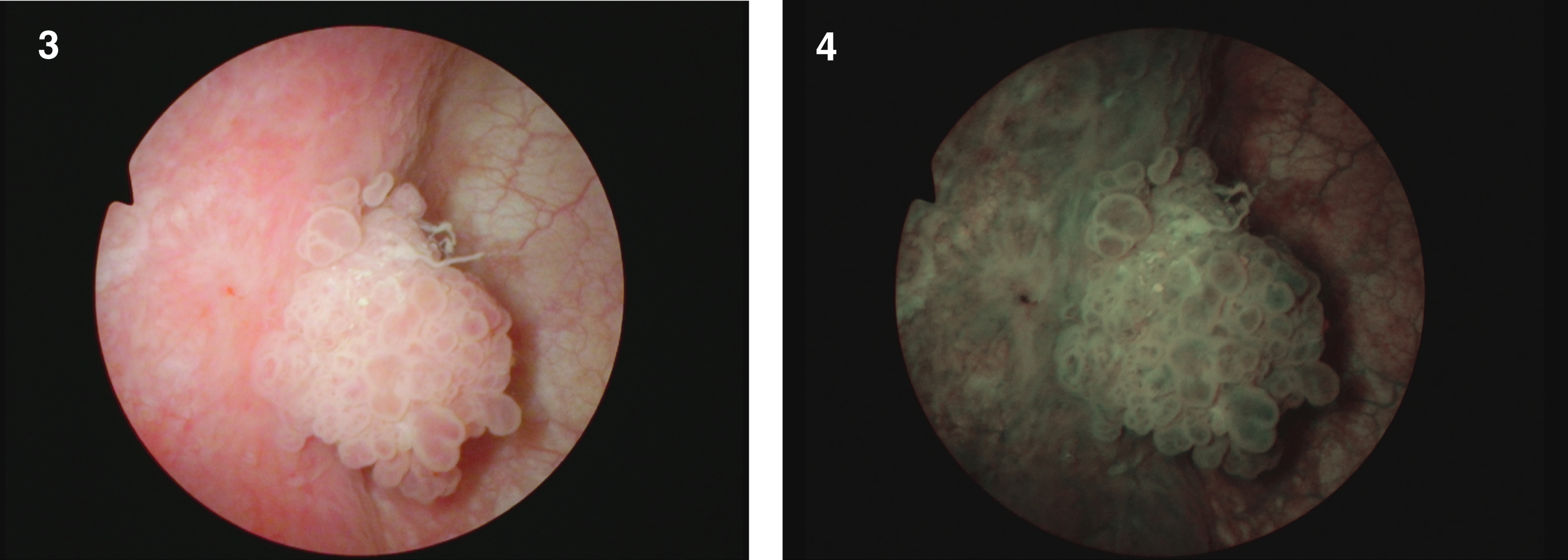
During the initial endoscopic exam under general anesthesia, I surveyed the bladder with a 30 and 70 degree lens using white light and NBI and did not identify any abnormalities other than the previously identified tumor. Figs. 3, 4. The TUR BT consisted of initial cold cup biopsies of the tumor and two erythematous areas adjacent to the tumor. A standard bipolar resection completed the tumor excision. There was no attempt to obtain muscle in the specimen as the cold cup biopsies were rather deep and excellent hemostasis was mandatory. The base of the resection was thoroughly cauterized with the button electrode.
Figs. 3-4
Papillary bladder cancer. White light and narrow band imaging.
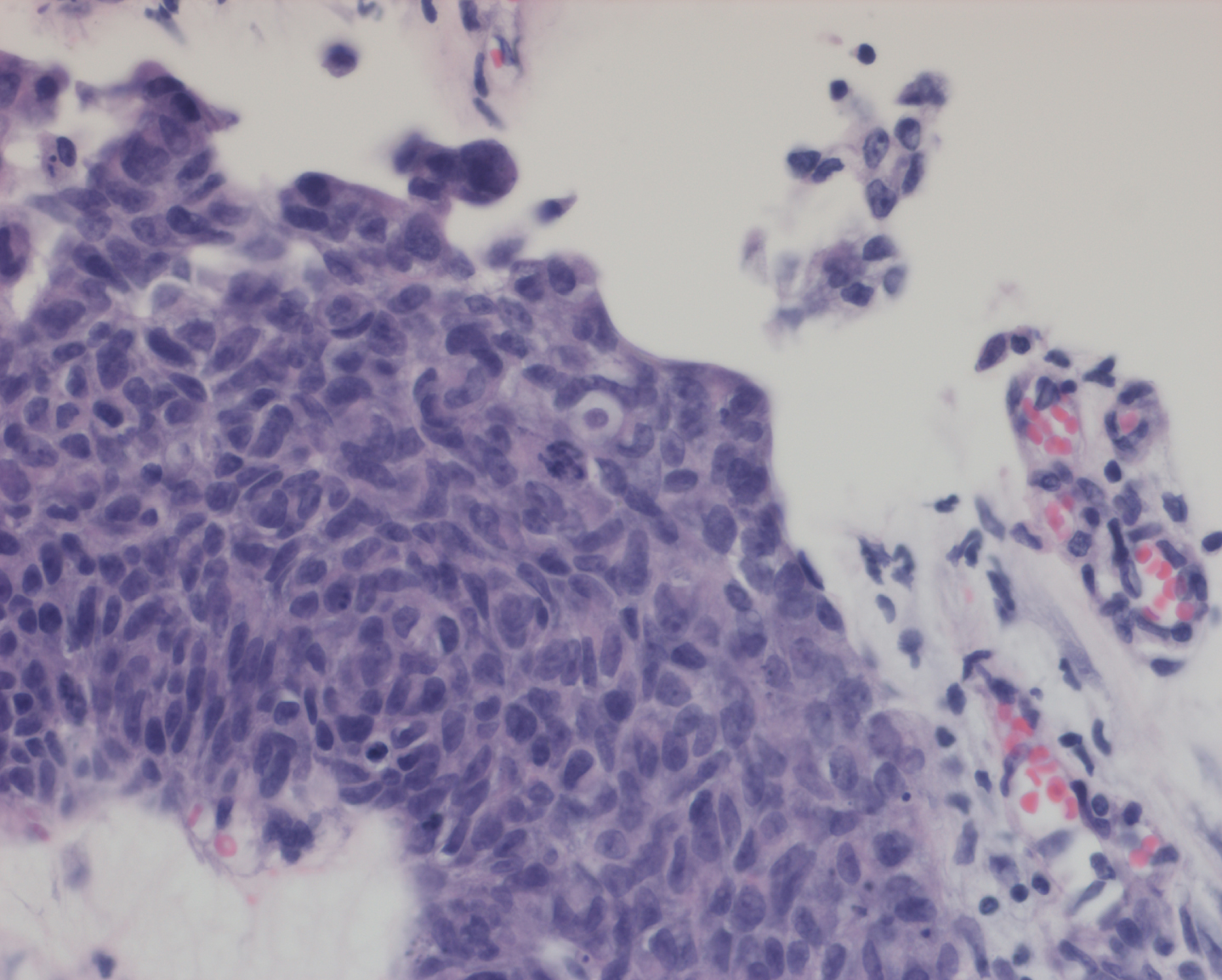
The pathology revealed a high grade urothelial carcinoma with minimal invasion of the lamina propria. There was no carcinoma in situ. Fig. 5.
Fig. 5
Papillary high grade urothelial carcinoma.
This is an unusual case in many ways. An incidental finding of a bladder tumor is unusual. The vast majority of patients with bladder cancer present with hematuria or voiding complaints. This woman has severe CHF and organ transplantation is an option. She does not appear ill as the LVAD allows her to go about her daily activities with minimal side effects.
One must contemplate the risk associated with immunosuppression should she have a transplant now versus the delay in performing the transplant. Importantly, as I have learned a patient can continue with the LVAD for years, if necessary, with only a modicum of risk.
I discussed intravesical BCG followed by the usual monitoring. I did not plan a re TUR BT because I felt confidant I removed all the tumor and there is an increased risk of perioperative morbidity with this patient.
I thought this case was quite unusual and was open to thoughts from colleagues with extensive experience in the treatment of bladder cancer and who may have had a similar case.
Sia Daneshmand and Roger Buckley advised no initial BCG but cystoscopy and cytology in 4– 8 weeks. If no new tumor proceed with transplant.
Fred Witjes indicated that if this were pTaLG proceed with the transplant but since she had a high grade T1a bladder cancer he would be reluctant to transplant before 1.5 years of being tumor free. He would start with intravesical mitomycin C.
Juan Palou suggested a re-TUR BT and if no invasive cancer begin intravesical BCG. If a heart became available before initiating the BCG he felt there is no problem giving an immunosuppressed patient BCG. Incidentally, I have given BCG to a few renal transplant patients who developed high grade Ta/T1/CIS bladder cancer in the years post-transplant. As I recall they did not have a complete response and had a cystectomy. There was no increase in local or systemic side effects however from the BCG.
Marc Colombel suggested using intravesical gemcitabine once no CIS is confirmed (she did not have CIS).
Maurizio Brausi suggested intravesical MMC with EMDA (not available in the US) or gemcitabine. He mentioned that the LVAD can be safely maintained for several months or longer if needed while the patient is being monitored. (There is some potential risks however, mainly infection or clotting).
Richard Hautmann would not give intravesical therapy now but have a strict surveillance protocol and local cautery for any small low grade appearing new tumor.
Ashish Kamat suggested intravesical chemotherapy with gemcitabine plus docetaxel.
Arnulf Stenzl would initiate optimization of mitomycin C. If no recurrence 3–6 months proceed to transplant.
Gaetano Ciancio (urologist and transplant surgeon) suggested to proceed with the heart transplant and then when she is a much better candidate for subsequent bladder cancer treatment proceed as needed depending on the grade and stage of any subsequent tumor.
Raj Persad also emphasized the importance of the heart transplant to her subsequent survival and would initiate intravesical therapy while waiting for the transplant.
Based in part on the above somewhat diverse expert opinions and having felt I removed all of the small unifocal bladder cancer, I initiated intravesical BCG. The initial cystoscopy after six weeks of BCG was normal with both white and narrow band imaging. Urine cytology was negative. She received three maintenance BCG doses.
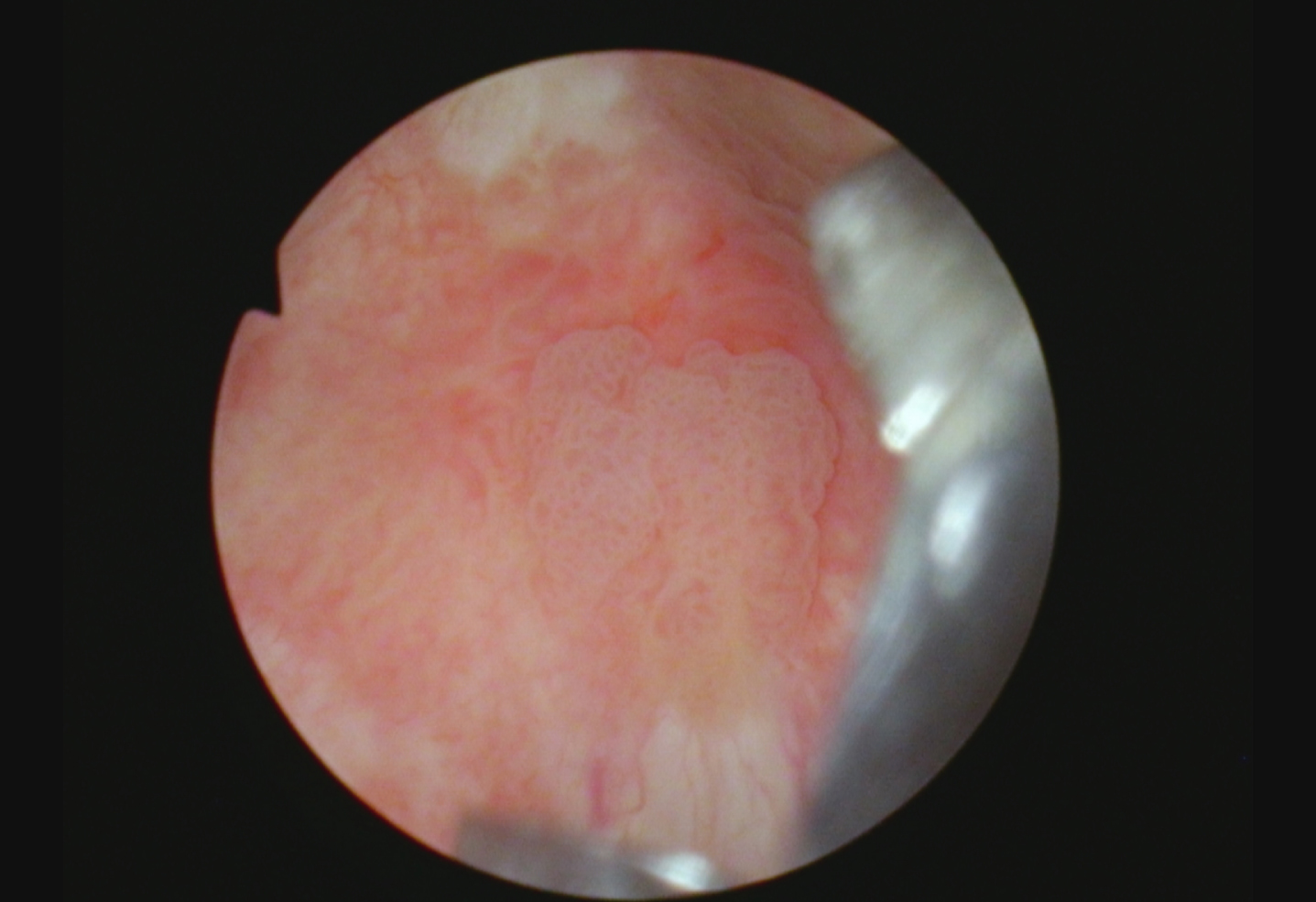
Nine months after the initial TUR BT the next flexible cystoscopy identified a small new tumor also on the left side of the bladder above the left ureteral orifice. It was small and appeared to be Ta. There was some surrounding erythema. I proceeded with a resection using cold cup biopsy to remove all of the small tumor and then thoroughly cauterized the resected base and the surrounding urothelium. Figs. 6, 7.
Fig. 6
Small papillary tumor.
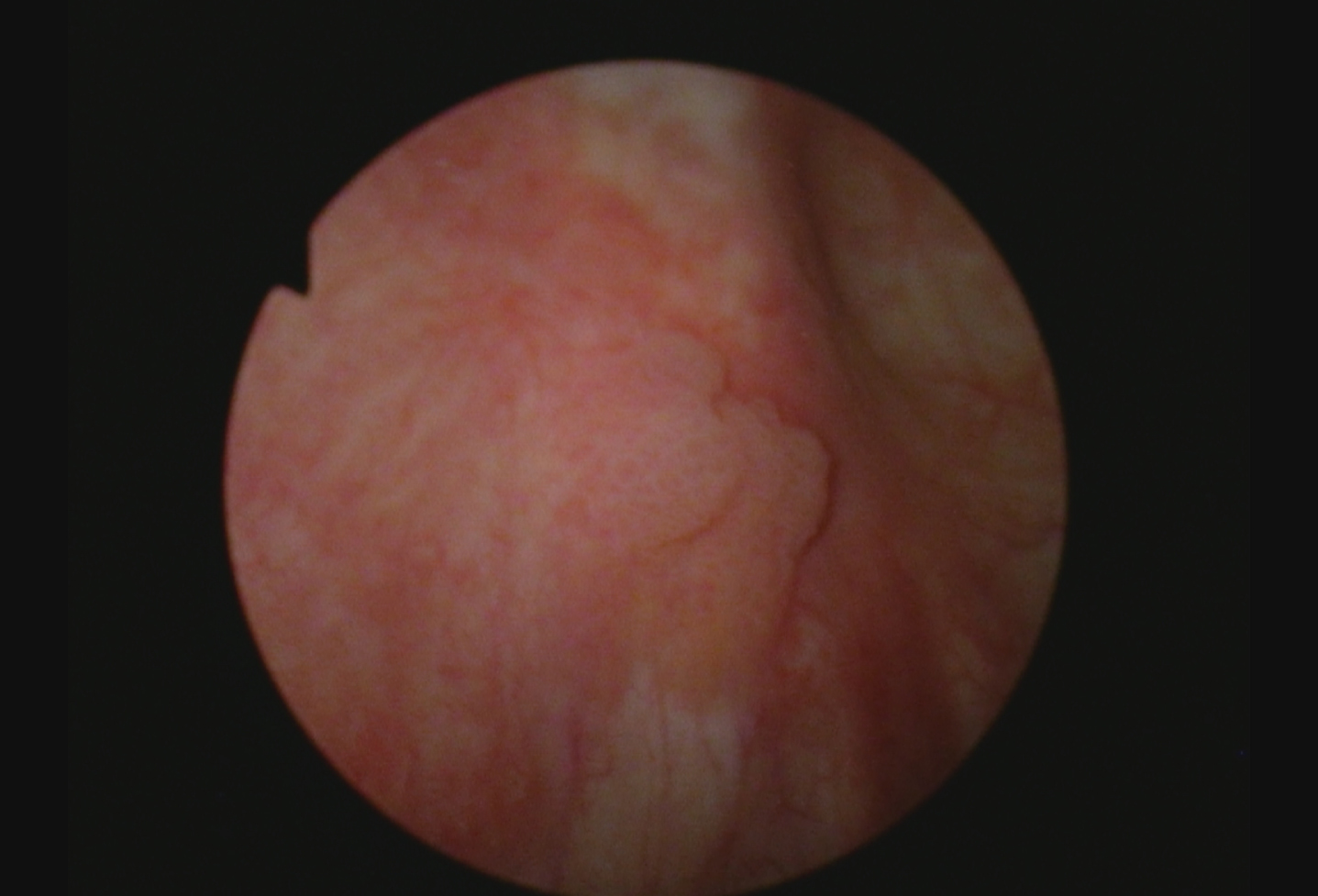
Fig. 7
Cold cup biopsy of the papillary tumor.
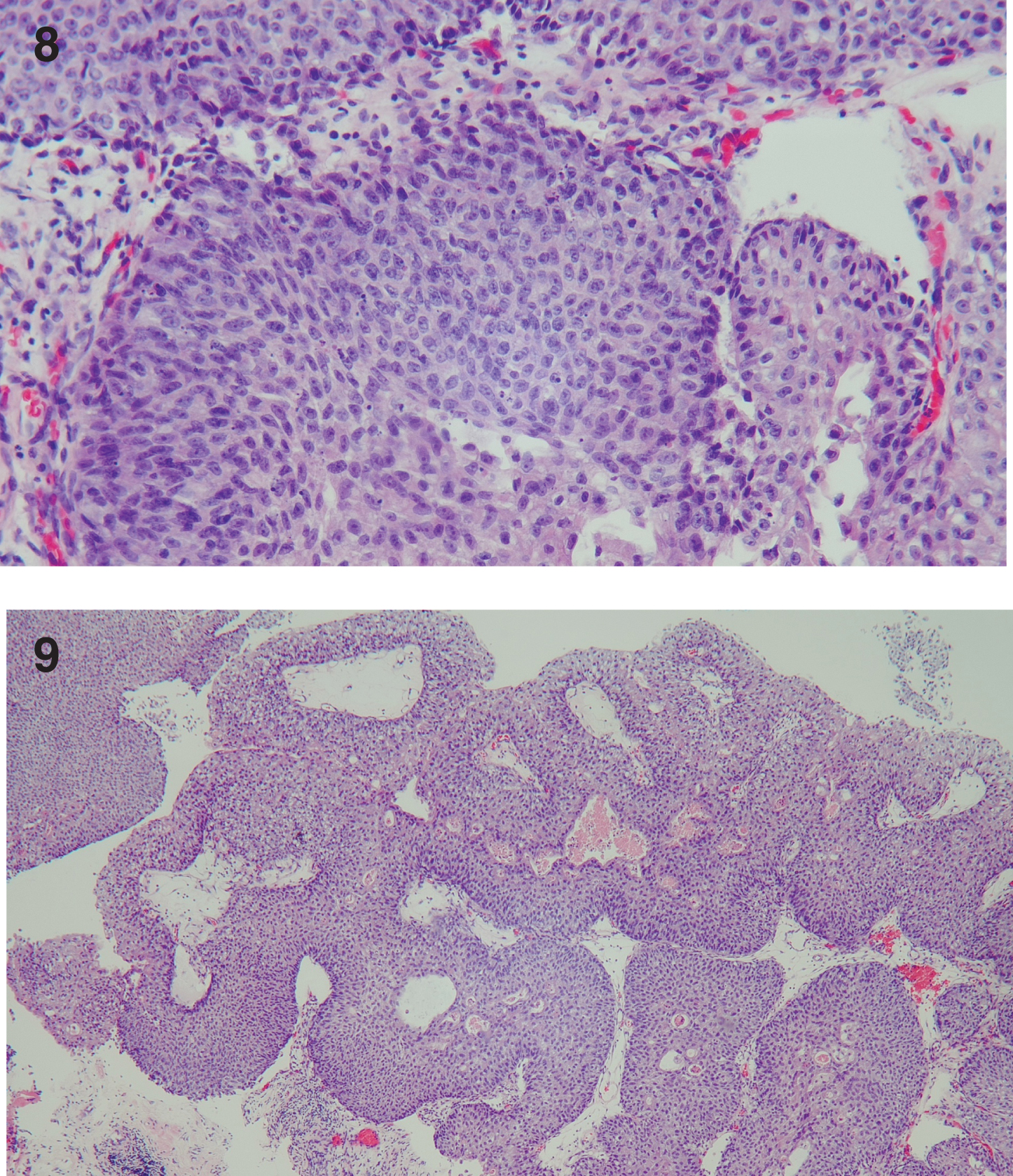
The pathology was high grade papillary Ta bladder cancer with inverted growth pattern and associated CIS. There was no invasion. Figs. 8, 9.
Figs. 8-9
High grade non invasive urothelial carcinoma with inverted growth pattern.
I once again reached out to my “consultants”. Harry Herr, Sia Daneshmand, Richard Hautmann, and Seth Lerner indicated another course of BCG would be reasonable before labeling her as BCG unresponsive. Seth would prefer a re-TURBT prior to the BCG to confirm she was tumor free prior to initiating the intravesical agent and to assess the rest of the urothelium for other areas of CIS. Sia indicated he would perform endoscopy and possibly a bladder biopsy after three doses rather than waiting the usual three months from initiating BCG.
Fred Witjes and Mauricio Brausi indicated their results with intravesical chemotherapy with hyperthermia and either mitomycin or gemcitabine are excellent, and this would be there choice now. Marc Columbel suggested intravesical gemcitabine and docetaxel.
Since patients with an LVAD can manage to do well for several years with this device Gaetano Ciancio and Richard Hautmann stressed that the status of her bladder cancer should be defined before the heart transplant.
I very much appreciated the opportunity to consult these colleagues and thank them for their prompt replies. I had a conference with the heart failure/transplant committee and indicated she will receive another course of BCG. I will not wait a full six weeks after the last dose to evaluate the bladder with cystoscopy and cytology.
AUTHOR CONTRIBUTIONS
MSS contributed to the work conception, performance, analysis of data and writing; NAA contributed to performance and analysis of data.
INFORMED CONSENT
Written informed consent for publication was obtained from the patient.
ETHICAL CONSIDERATIONS
The author has institutional review board approval for reviewing bladder cancer cases for outcome (MHS.2020.026).
CONFLICT OF INTEREST
MSS and NAA have nothing to disclose.




