Challenging Cases in Urothelial Cancer: Case 26
This 37 year old healthy appearing man had a seven month history of intermittent gross hematuria. He has no voiding problems beside hematuria. He has hypertension and takes losartan and hydrochlorothiazide. He has not had surgery. He has never smoked cigarettes or cigars.
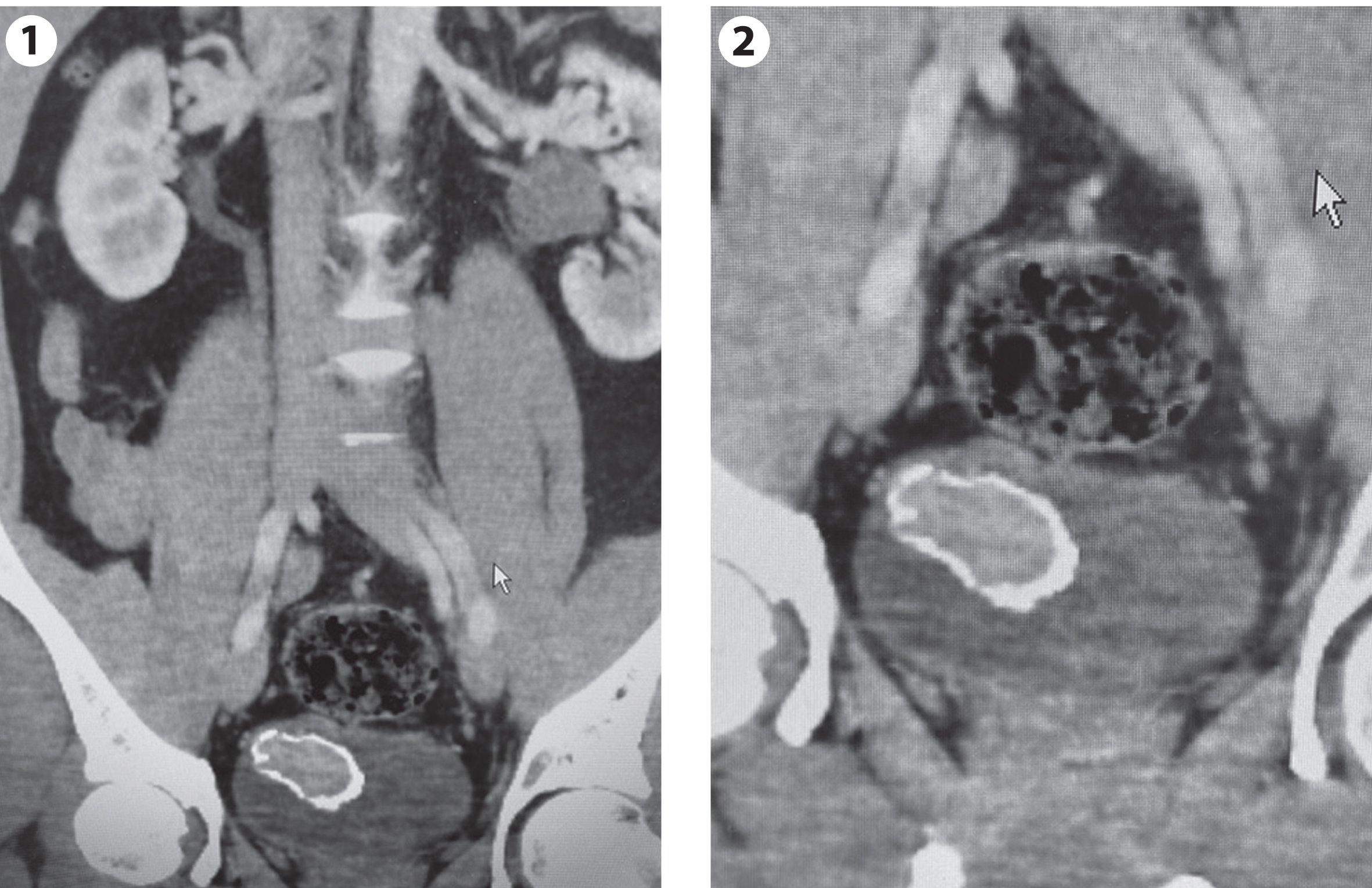
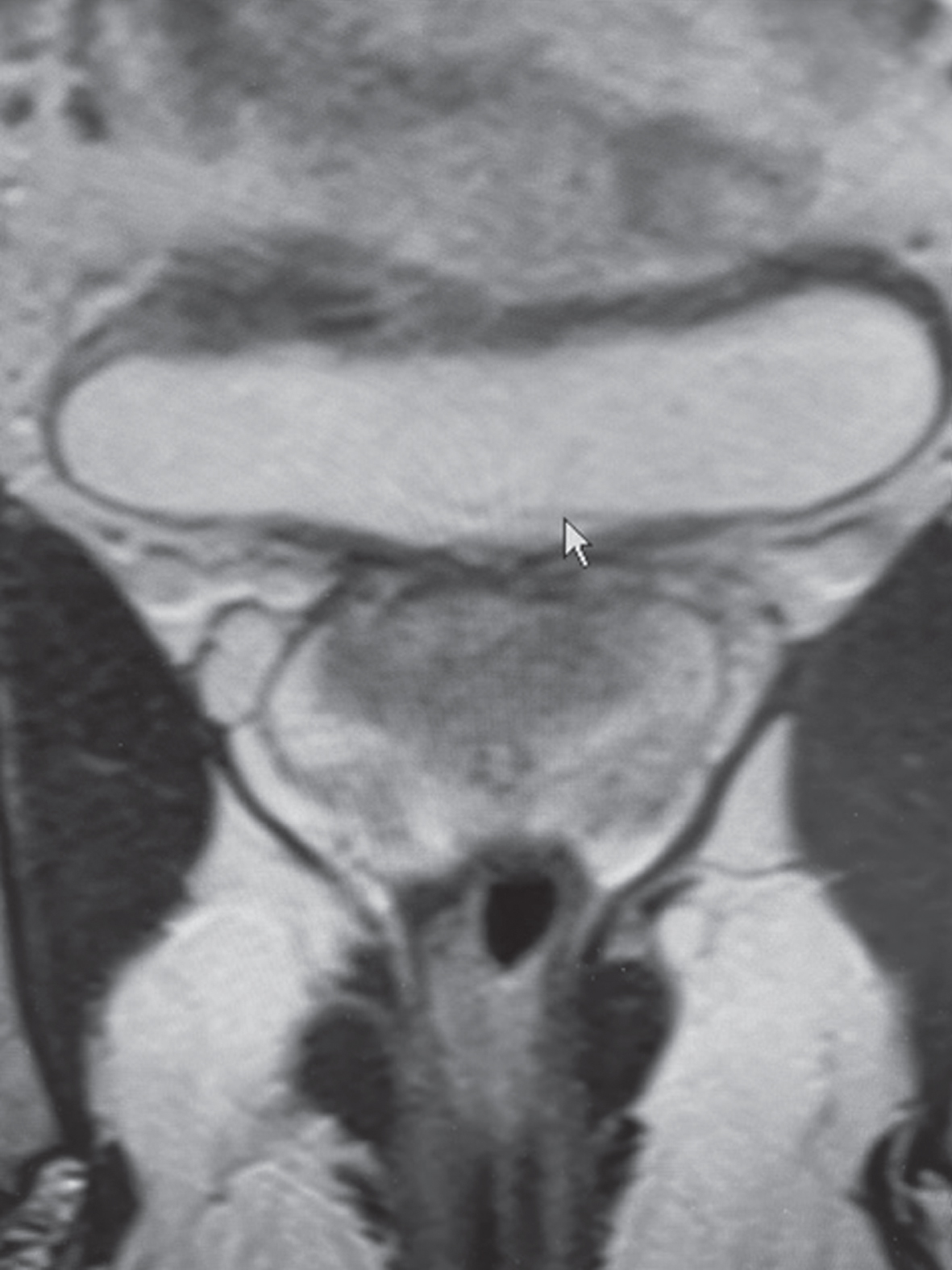
He was initially evaluated by a urologist in March 2022. A CT scan of the abdomen and pelvis indicated a normal upper urinary tract however the bladder contained a 3.8×2.5×2.5 cm partially calcified mass located in the posterior lateral wall which was thought to be a bladder calculous (Fig. 1-2). During a flexible cystoscopy the mass was identified as a bladder tumor.
Fig. 1-2
CT scan indicating a calcified mass of about 4 cm.
He underwent a transurethral resection of the bladder tumor (TUR BT) in April 2022. The operative report indicated a solitary, large, partially calcified tumor located in the anterolateral wall. The urologist operative note stated that he performed a “complete” resection and that he obtained “deep bites for adequate staging". The pathology report stated that this was a high grade papillary urothelial carcinoma with at least invasion into the lamina propria, HG T1. There was no muscle in the specimen. There was calcification and extensive cautery artifact.
I initially evaluated the patient in April 2022 and explained that according to the AUA/SUO and EAU guidelines for NMIBC a repeat TUR BT is indicated after an initial resection of a HG T1 bladder cancer (BC). On the morning of the planned re TUR BT the patient awoke with significant gross hematuria and came to the emergency department where a three-way urethral catheter was placed for continuous irrigation. Since the TUR BT was scheduled that same today and the patient was compliant with not eating the night before the procedure he was transferred to the operating room.
After endotracheal general anesthesia was induced, I placed a 27 Fr Iglesias resectoscope into the bladder and evacuated numerous blood clots. Once the clots were removed the prior resection site was identified high on the right lateral wall (Fig. 3-4). There was minimal bleeding. Using the bipolar resectoscope I proceeded with a re TUR BT of the prior resection site and thoroughly cauterized the entire area with the button electrode (Fig. 5). The pathology was carcinoma in situ (CIS), no invasive tumor (Fig. 6-7).
Fig. 3-4
Area of prior resection on the posterior lateral wall.
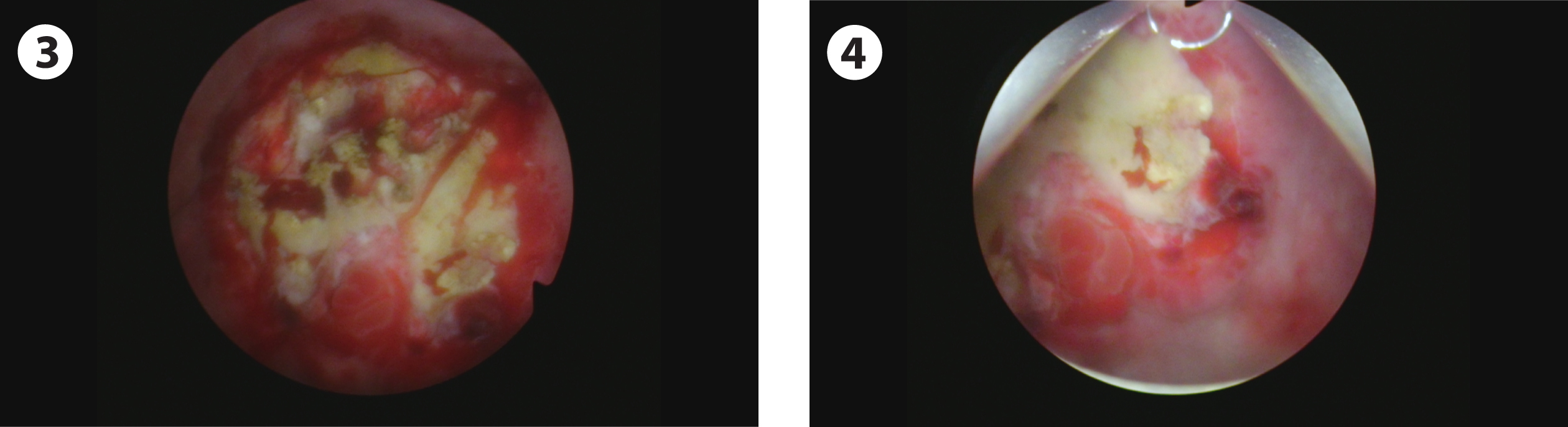
Fig. 5
Post resection after cautery.
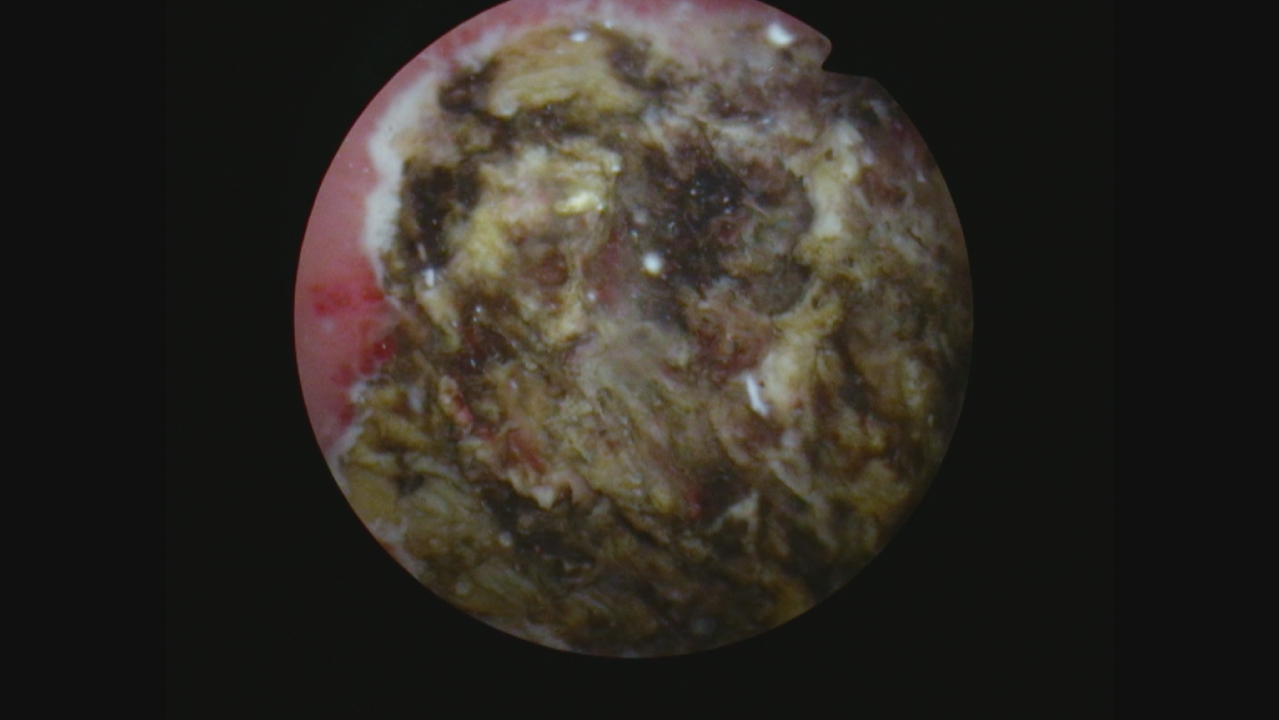
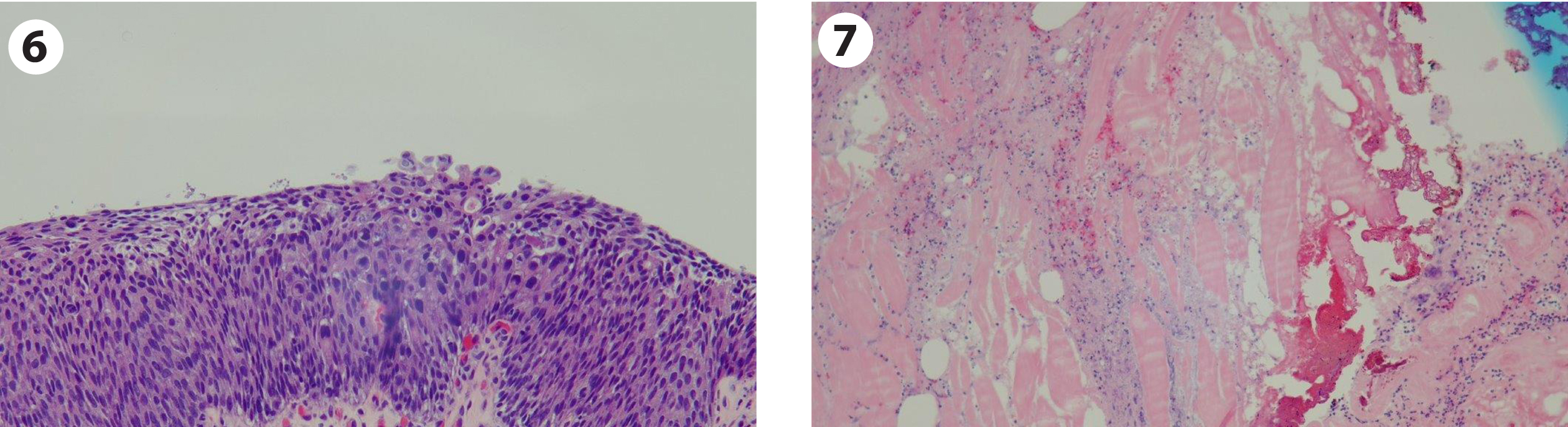
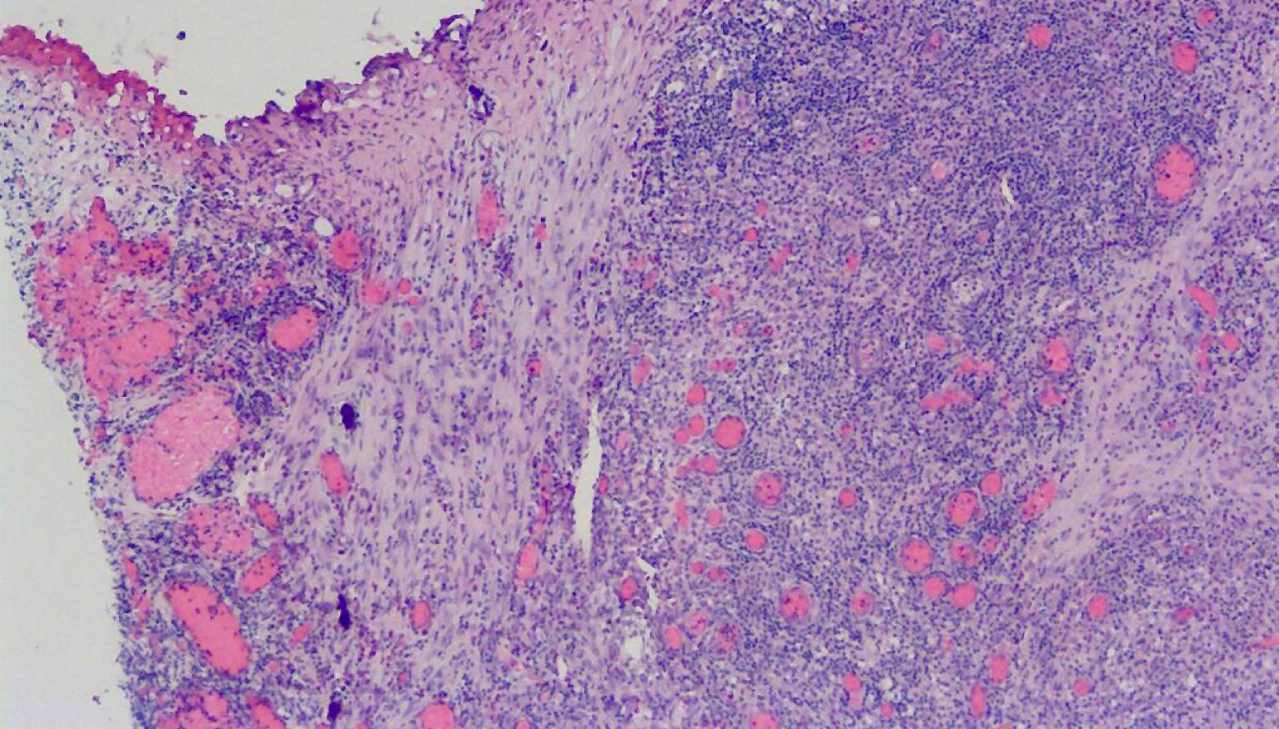
Fig. 6-7
Pathology indicating carcinoma in situ and no tumor in the lamina propria or muscle.
I considered several alternatives. I was concerned about the initial imaging which identified a mass which appeared to represent a possible muscle invasive bladder cancer. The initial cancer was HG T1 and on re resection was CIS. The guidelines state that in some circumstances an otherwise healthy patient with HG T1 plus CIS can be considered for a radical cystectomy. Of course, the alternative would be BCG if convinced there is no muscle invasive cancer.
I proceeded with a six week course of BCG after discussing these alternatives with the patient and family. His age, 37 years old, was certainly a major factor and was considered in a discussion both for and against removing the bladder.
An MRI was performed in May 2022 (Fig. 8). The interpretation was a “lesion involving the right lateral wall with features concerning for muscle invasion, no perivesical extension". The radiologist indicated the lesion measured 1.7×1.5 cm. “There is interruption of the low signal intensity of the muscularis propria concerning for possible muscle invasion. On the post contrast sequences the lesion appears to be confined without invasion of the perivesical fat.” There was no lymph node enlargement.
Fig. 8
MRI indicating a small area of thickening of the bladder wall with an invasive bladder cancer being one of the alternatives.
In July 2022 I performed the first post BCG flexible cystoscopy and bladder wash cytology. There was an area of altered urothelium at the prior cancer location. The initial tumor was solitary and, not surprisingly, the rest of the bladder was normal. The cytology indicated only suspicious cells.
Given my concern about the MRI report along with the suspicious area in the bladder, I proceeded with transurethral resection of this area using both white and narrow band imaging during the course of the procedure. I initially obtained cold cup biopsies from normal appearing urothelium and then performed an en bloc TUR BT with the standard right angle bipolar loop which I bent to conform it to the curve of the bladder wall (Fig. 9–12). The pathology indicated no cancer in any of the tissue (Fig. 13). He is receiving maintenance BCG.
Fig. 9
Endoscopic appearance of the abnormal urothelium in the location of the prior cancer location.
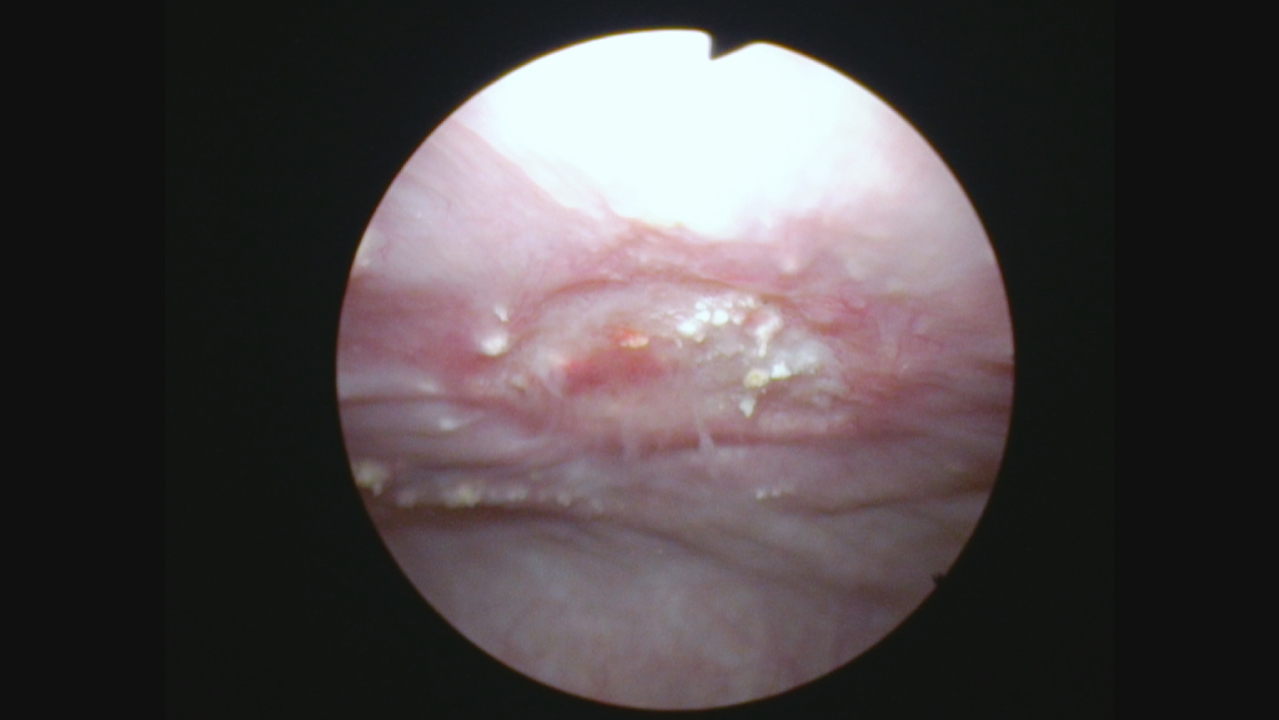
Fig. 10
Narrow band imaging appearance of this same area suspicious for tumor.
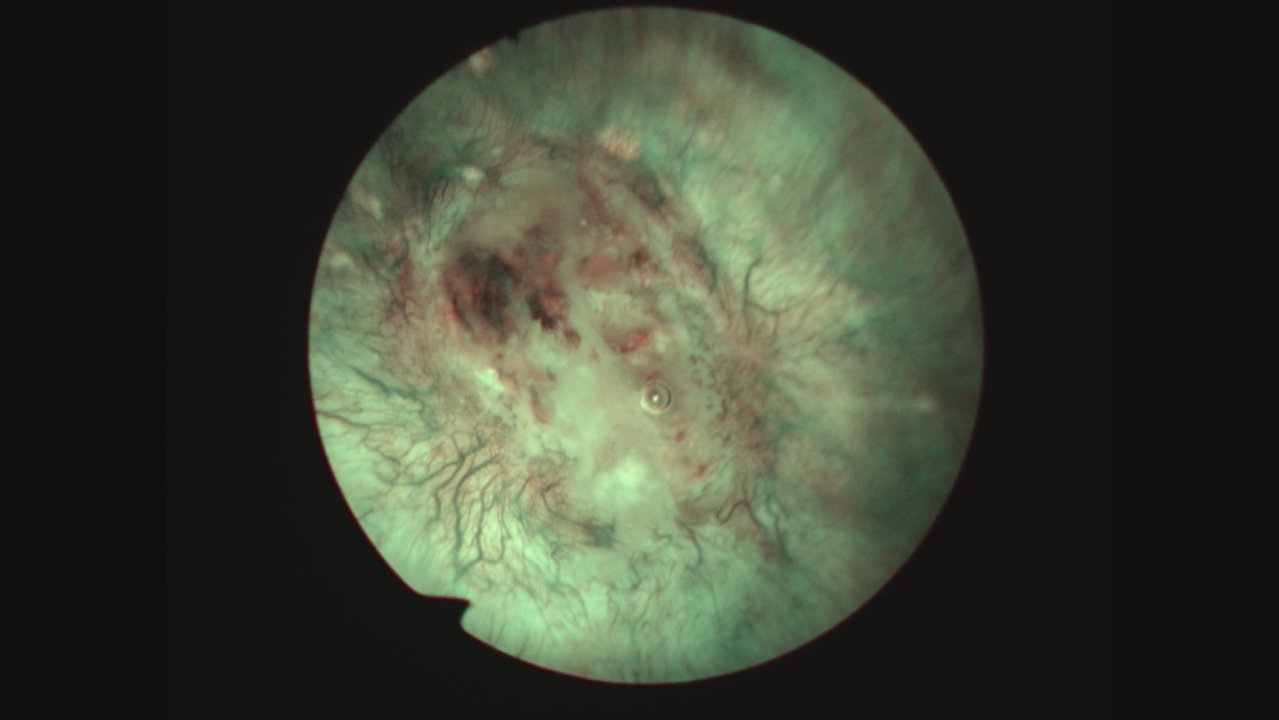
Fig. 11
En bloc resection of this abnormal area.
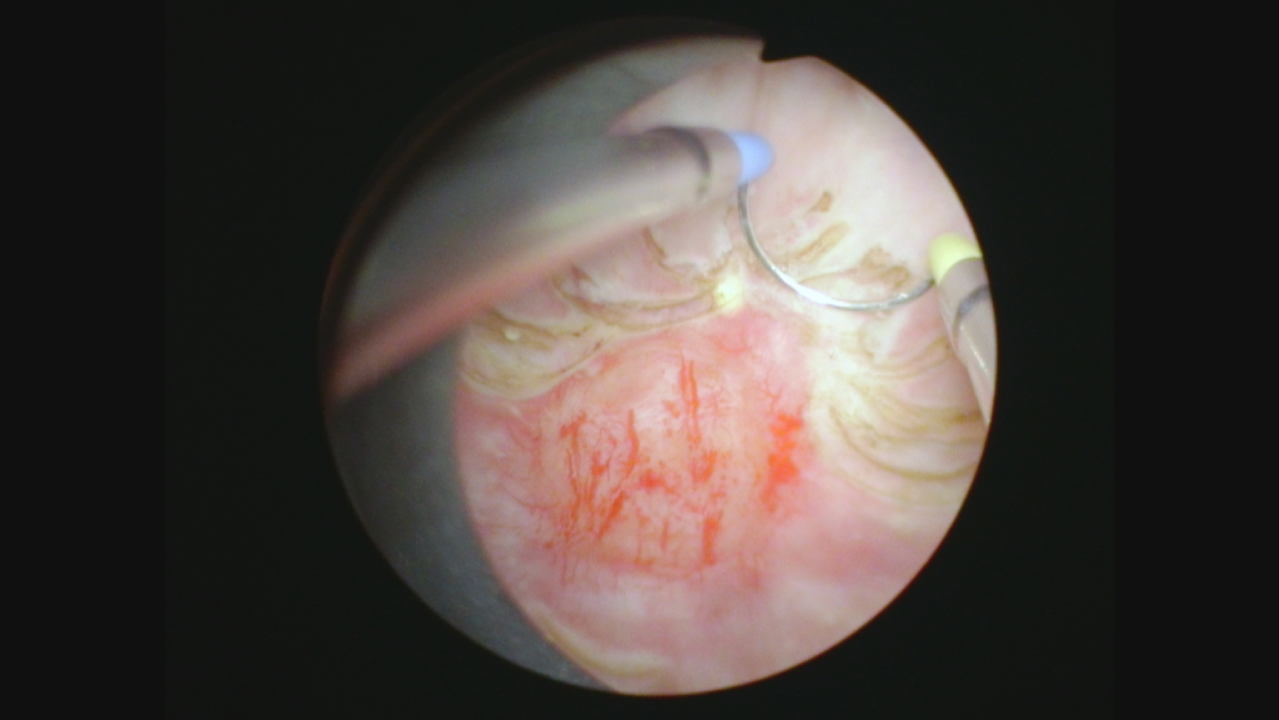
Fig. 12
View of the area following the repeat TUR BT identifying deep muscle without any appearance of bladder cancer.
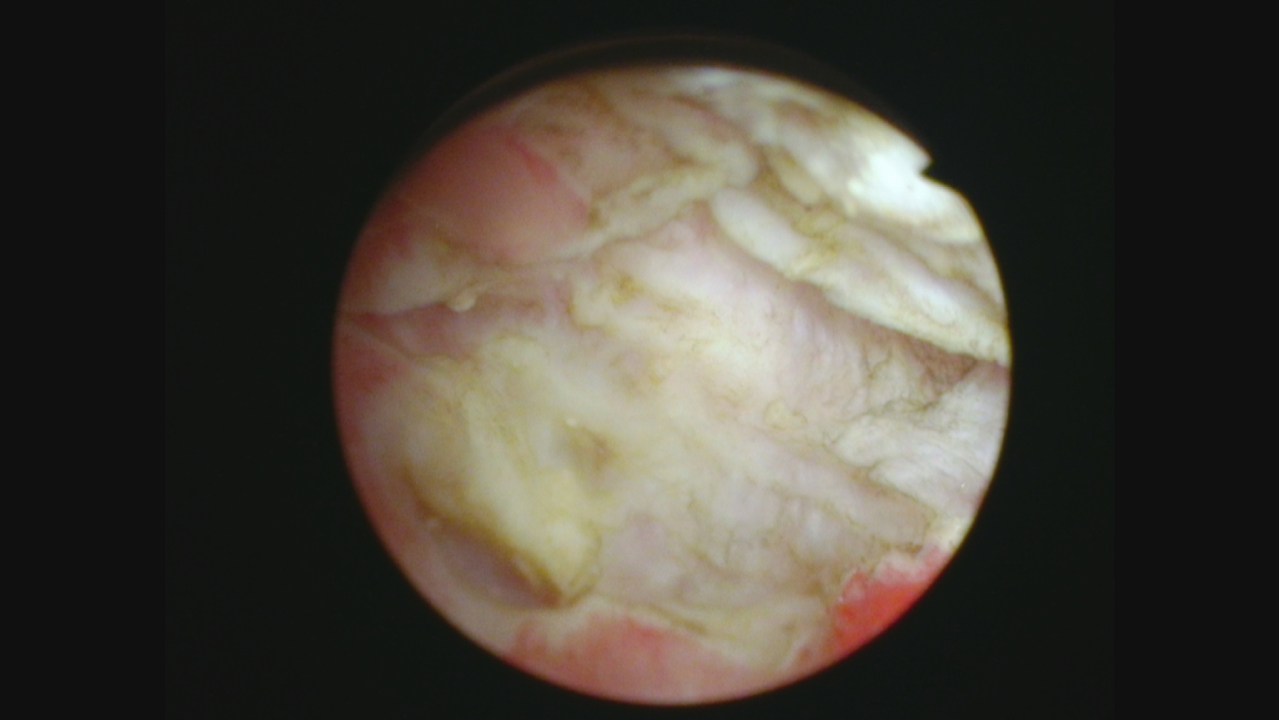
Fig. 13
Pathology of the repeat resection showing no cancer; chronic inflammation only.
This case was particularly challenging given his age at presentation and the images of the bladder on the initial CT and subsequent MRI. I am convinced he did not have a muscle invasive urothelial cancer.
The diverse opinions regarding management of HG T1 BC can be illustrated by a recent second opinion consultation for a 47 year old healthy appearing man. He had a screening abdominal/pelvic ultrasound as a part of routine comprehensive physical exam provided by his company. He had a few episodes of gross hematuria which were limited and he had not sought care. He never smoked. Due to Covid restrictions there was a delay in his seeking care. An initial urology visit led to a cystoscopy and the finding of a large bladder cancer. He was then evaluated by a urologic oncologist. In December 2021 he had a TUR BT of a moderately large papillary urothelial tumor. The initial pathology report stated that this was a muscle invasive cancer but a separate review of the material stated muscle was present but not invaded. A repeat TUR three weeks later revealed no cancer. He received BCG weekly for 6 weeks then monthly for several months. In January, April, and August 2022 he was found to have small papillary low grade Ta tumors. All were < 1 cm. The number ranged from 1–3. In each case a formal TUR BT was performed. The urologic oncologist recommended a cystectomy because of his age and new tumors despite BCG. The patient sought another opinion and this urologist recommended intravesical mitomycin C and pembrolizumab. I told the patient that, in my opinion, small LG Ta appearing tumors could be potentially cauterized in the office. I did not advise additional BCG, a cystectomy or systemic immunotherapy.
INFORMED CONSENT
Written informed consent for publication was obtained from the patient.
ETHICAL CONSIDERATIONS
The author has institutional review board approval for reviewing bladder cancer cases for outcome (MHS.2020.026).
CONFLICT OF INTEREST
Nothing to disclose.




