Physical Activity and Health-related Quality of Life from Diagnosis to One Year After Radical Cystectomy in Patients with Bladder Cancer: A Longitudinal Cohort Study
Abstract
BACKGROUND:
Emerging evidence shows a positive impact of physical activity (PA) on health-related quality of life (HRQoL) in cancer patients. However, longitudinal evidence on PA and HRQoL in patients with bladder cancer (BC) undergoing radical cystectomy (RC) is lacking.
OBJECTIVES:
To investigate PA levels, HRQoL outcomes and their relationship from diagnosis to one year after RC in BC patients.
METHODS:
A longitudinal cohort study in 90 BC patients was conducted at Ghent and Leuven University Hospitals between April 2017 and December 2020. The Godin Leisure-Time Exercise Questionnaire (GLTEQ) and the EORTC QLQ-C30 and BLM30 were used to measure PA and HRQoL, respectively, before RC, one, three, six and twelve months after RC. Linear mixed models were used for statistical analyses.
RESULTS:
The majority was physically inactive before RC (58%), at month one (79%), three (53%), six (61%) and twelve (64%). Among (moderately) active patients, light-intensity activities (mainly walking) were important contributors to the total amount of PA. Clinically important and low HRQoL outcomes in different domains were identified with lowest scores at diagnosis and one month after RC. Active patients before RC have better physical functioning (mean difference (MD) -22.7, standard error (SE) 8.7, p = 0.011), global health status (MD -15.9, SE 6.9, p = 0.023) and fatigue (MD 19.9, SE 9.5, p = 0.038) one month after RC, compared to inactive patients. Active patients at month have better physical functioning (MD -16.2, SE 6.9, p = 0.023) and sexual functioning (MD -16.8, SE 5.4, p = 0.003; MD -13.5, SE 5.5, p = 0.017) at month six and twelve, respectively, compared to inactive patients.
CONCLUSIONS:
Higher PA levels are associated with better HRQoL outcomes for BC patients undergoing RC. The data suggests that PA interventions could be an asset to improve BC patients’ HRQoL, but should be tested in future trials.
INTRODUCTION
Radical cystectomy (RC) with the construction of a new urinary diversion is an invasive treatment which severely impacts different health-related quality of life (HRQoL) domains in patients with bladder cancer (BC) [1]. Evidence showed that BC patients undergoing RC experience several disease- and treatment-related side-effects (e.g. urinary and sexual dysfunctions, fatigue, psychological distress) which contribute to a lower functional status (e.g. physical, mental, social) [2]. Two recent studies show that patients undergoing RC experience declines in HRQoL up to three months after RC, but improve again after three months [3, 4]. Since BC is mainly diagnosed in the elderly, advanced age and associated comorbidities contribute to physical and psychosocial declines [5]. Furthermore, BC patients show lower levels of physical activity (PA) and worse general health perceptions compared to the general population [6].
In the past decade, emerging evidence showed that PA improves the physical and psychosocial condition among cancer patients. More specifically, cancer patients engaging in sufficient PA showed better HRQoL outcomes in several domains (e.g. treatment-related side-effects, physical functioning) compared to non-active peers [7]. In addition, evidence showed beneficial effects of preoperative PA interventions (also known as ‘prehabilitation’) on postoperative outcomes for patients undergoing major intra-abdominal cancer surgery [8]. So far, only four PA trials were conducted in BC patients before or after RC and showed that PA improves physical fitness, muscle strength and some HRQoL domains (e.g. activities of daily living) [9, 10].
The current body of evidence described in the previous paragraph is mainly based on studies investigating moderate- to vigorous-intensity PA [7] which prompted the development of PA guidelines by the American College of Sports Medicine (ACSM): at least three times a week moderate-intensity aerobic activity for 30 minutes and twice-weekly resistance exercises [11]. However, emerging evidence also suggests benefits of light-intensity PA for mortality, cardiometabolic risk factors, and physical health, especially in an elderly and frail cancer population [12]. Promoting light-intensity activity in BC patients might be a successful strategy since light-intensity activities such as walking are more realisable for older adults with multiple comorbidities [13].
So far, longitudinal evidence on changes in PA (of any intensity) and HRQoL and the effect of PA on HRQoL in BC patients undergoing RC is lacking. This information is important to inform the design and tailoring of future PA interventions for BC patients. Therefore, the objectives of this study were to describe HRQoL (and its clinical relevance) and PA levels from diagnosis to one year after RC. Furthermore, this study aims to investigate how early PA levels impact later HRQoL outcomes. More specifically, this research aims to investigate how preoperative PA levels can predict HRQoL outcomes at month one and three after RC and how PA levels at month three after RC can predict HRQoL outcomes at month six and twelve after RC. These choices were made because we want to understand the impact of PA in the preoperative setting and the early postoperative setting to develop future prehabilitation and early postoperative recovery PA programs for BC patients.
METHODS
Study design
A multicentre longitudinal cohort study was conducted with survey measurements scheduled before RC (four weeks before RC) (T1), one month (T2), three months (T3), six months (T4) and twelve months after RC (T5). The study protocol was registered at clinicaltrials.gov (NCT03307200) and approved by the ethical committee of Ghent University Hospital (EC/2017/1362) and University Hospital Leuven (S61059).
Participants
Patients were eligible if they were aged 18 + years, diagnosed with BC and scheduled for open or robotic RC at Ghent University Hospital or the University Hospital Leuven, metastasis free at diagnosis, free of a second primary tumour at diagnosis (except for removed prostate cancer or non-melanoma skin tumour and a tumour diagnosed more than five years ago and being under control), and were capable to sign and understand the informed consent.
Data collection and measurements
Patients were recruited at the Urology departments from Ghent University Hospital and the University Hospital Leuven between April 2017 and December 2019 where they gave written informed consent. Data collection was completed in December 2020.
Demographic and clinical predictors
Demographic and clinical data were collected with the use of a case report form. The following variables were collected: age, sex, marital status, educational level, work status, body mass index (BMI), smoking status, familial history of cancer, medication use, comorbidities according to the Charlson comorbidity index and treatment-related variables such as administration of neoadjuvant chemotherapy and type of urinary diversion. This case report form was completed at baseline by the patients. Clinical recurrence and death within the first year after radical cystectomy was collected via chart review. If patients received adjuvant treatments after radical cystectomy, this information was also collected via chart review and added by the research team. In addition, health literacy (i.e. the ability to obtain, read, understand and use healthcare information) was measured with the BRIEF health literacy screening tool, which is a validated four-item instrument to measure health literacy.
Physical activity levels
The Godin Leisure-Time Exercise Questionnaire (GLTEQ) is a validated tool in oncology research and was used to measure PA levels [14]. The GLTEQ assesses the average frequency of leisure-time light, moderate, and vigorous PA for at least 15 minutes in a typical seven-day week. Note that the questionnaire does not account for the length of each PA session as it assesses the frequency of PA periods of at least 15 minutes. Light-intensity PA requires a minimal effort and include activities such as fishing, golf, and easy walking. Moderate PA includes activities that are not exhausting such as fast walking, tennis, easy cycling, and easy swimming. Vigorous PA includes activities in which the heart beats rapidly such as running, jogging, playing football, vigorous swimming, and vigorous cycling.
The weekly frequencies of light, moderate, and vigorous PA were then multiplied by metabolic equivalents (3, 5, 9, respectively) and summed to form a total score of leisure time PA. According to the proposed original categories by Godin [14], the total score (including light intensity PA) was then subdivided into patients who are insufficiently active (<14), moderately active (14–23) and active (≥24).
Health-related quality of life
Cancer-specific HRQoL is measured with the validated HRQoL questionnaire of the European Organization for Research and Treatment of Cancer (EORTC QLQ-C30) [15]. The questionnaire includes five functional scales (physical, emotional, role, social, and cognitive functioning), nine cancer-related symptom scales (fatigue, nausea and vomiting, pain, dyspnoea, insomnia, appetite loss, constipation, diarrhoea and financial difficulties) and a global health status scale. In addition, BC specific HRQoL was measured with the muscle-invasive bladder cancer module (EORTC QLQ-BLM30). This is a 30-item questionnaire assessing urinary or urinary diversion related symptoms, bowel symptoms, body image, future perspectives and sexual functioning.
Published thresholds for clinical importance will be used to interpret the results from the EORTC QLQ-C30 [16].
Statistical analyses
Statistical analyses were performed in SPSS Statistics 25. Descriptive statistics were used to describe the sample characteristics. The EORTC manual was used for dealing with missing HRQoL data and appropriate scoring of the HRQoL data. The numbers (ranging from 1 to 4 on a Likert-scale) were converted into values ranging from 0 to 100. A score of 100 can be interpreted as maximal function (e.g. emotional functioning) or maximal symptoms (e.g. fatigue).
Mean scores, 95% confidence intervals, changes in PA and HRQoL outcomes and relationships between PA and HRQoL outcomes were calculated using linear mixed-effect models with autoregressive variance-covariance structure. Relationships between PA and HRQoL were only examined for HRQoL outcomes where we hypothesized PA could have a benefit. Therefore, the following HRQoL outcomes were used for the purpose to investigate the relationship between PA and HRQoL: physical functioning, emotional functioning, fatigue, global health status, sleep disturbances, and sexual functioning. Furthermore, we chose to investigate the relationship between 1) preoperative PA and HRQoL at month one and three after RC and 2) PA at month three after RC and HRQoL at month six and twelve after RC.
The linear mixed-effect models were adjusted for demographic and clinical variables that showed significant associations with PA across time-points. Significant associations were explored with univariate analyses. Independent if age was significantly associated with PA or not, we adjusted for age in the analyses as age has shown to be an important contributor to PA and HRQoL in the literature [17]. Participants were divided into ‘younger’ (<65 years) and ‘older’ (≥65 years) age groups for the analyses. The age of 65 is frequently used as cut-off to define older age.
RESULTS
In total, 103 eligible patients were invited to participate of which 90 patients (response rate of 87%) were willing to be included in this longitudinal study. The percentage of missing data for PA was 4%, 9%, 20%, 27% and 35% at baseline, month one, three, six and twelve, respectively. The percentage of missing data for HRQoL was 5%, 18%, 23%, 22% and 30% at baseline, month one, three, six and twelve, respectively. Missing data was partly due to patient withdrawal (n = 5), disease progression (n = 2) and death of participants (n = 10). Other reasons for missing data were: patients not sending back the questionnaire with unknown reason, administrative failure, patients returning a blank questionnaire, concentration problems, and not willing to complete the questionnaire.
Demographic and clinical patient characteristics are presented in Table 1.
Table 1
patient characteristics (N = 90)
| Demographical information | Preoperative PA levels | ||||
| Insufficient active | Moderately active | Active | p-value | ||
| Gender: n(%) | .236 | ||||
| Men | 74 (83%) | 39 (55%) | 19 (27%) | 13 (18%) | |
| Women | 16 (17%) | 11 (73%) | 1 (7%) | 3 (20%) | |
| Age (Mean±SD) | 69±10 | 70±9 | 67±12 | 67±13 | .373 |
| Marital status: n(%) | .496 | ||||
| Married or living as married | 66 (73%) | 40 (62%) | 14 (22%) | 10 (16%) | |
| Not married | 17 (19%) | 9 (54%) | 4 (23%) | 4 (23%) | |
| Missing | 7 (8%) | ||||
| Education level: n(%) | .414 | ||||
| Primary school | 13 (14%) | 9 (69%) | 2 (15%) | 2 (15%) | |
| Secondary school | 36 (40%) | 21 (60%) | 10 (29%) | 4 (11%) | |
| Bachelor’s degree | 18 (20%) | 10 (56%) | 4 (22%) | 4 (22%) | |
| Master’s degree | 10 (11%) | 6 (60%) | 1 (10%) | 3 (30%) | |
| Other | 1 (1%) | 0 | 0 | 1 (100%) | |
| Missing | 12 (13%) | ||||
| Employment status: n(%) | .145 | ||||
| Full-time | 10 (11%) | 3 (33%) | 5 (56%) | 1 (11%) | |
| Part-time | 2 (2%) | 2 (100%) | 0 | 0 | |
| Retired | 66 (73%) | 42 (65%) | 12 (18%) | 11 (17%) | |
| Volunteering work | 5 (6%) | 2 (40%) | 1 (20%) | 2 (40%) | |
| Missing | 7 (8%) | ||||
| BMI: n(%) | .700 | ||||
| Underweight (<18.5) | 17 (19%) | 11 (65%) | 3 (18%) | 3 (18%) | |
| Normal weight (18.5-24.99) | 49 (54%) | 29 (60%) | 10 (21%) | 9 (19%) | |
| Overweight (≥25) | 13 (15%) | 6 (46%) | 5 (38%) | 2 (15%) | |
| Missing | 11 (12%) | ||||
| Smoking status: n(%) | .169 | ||||
| Non-smoker | 21 (23%) | 8 (40%) | 7 (35%) | 5 (25%) | |
| Smoker | 15 (17%) | 10 (67%) | 4 (27%) | 1 (7%) | |
| Ex-smoker | 43 (48%) | 29 (67%) | 6 (14%) | 8 (19%) | |
| Missing | 11 (12) | ||||
| Clinical and treatment information | |||||
| Charlson Co-morbidity index (mean±SD) | 5.8±1.8 | 6.0±1.7 | 5.5±1.9 | 5.2±1.8 | .309 |
| Pathological T-stage: n(%) | .581 | ||||
| Ta-Tis | 8 (9%) | 5 (71%) | 1 (14%) | 1 (14%) | |
| T1 | 9 (10%) | 3 (33%) | 2 (22%) | 4 (44%) | |
| T2 | 27 (30%) | 18 (67%) | 5 (18%) | 4 (15%) | |
| T3 | 28 (31%) | 15 (58%) | 7 (27%) | 4 (15%) | |
| T4 | 9 (10%) | 5 (56%) | 3 (33%) | 1 (11%) | |
| Urinary diversion type: n(%) | |||||
| Ileal conduit | 64 (71%) | ||||
| Neobladder | 25 (28%) | ||||
| Mainz Pouch | 1 (1%) | ||||
| Neoadjuvant chemotherapy: n(%) | 46 (51%) | 25 (58%) | 10 (23%) | 8 (19%) | .941 |
| Adjuvant radiotherapy: n(%) | 23 (26%) | 10 (45%) | 8 (36%) | 4 (18%) | .182 |
| Clinical recurrence within the first year after radical cystectomy (n(%)) | 19 (21%) | 8 (44%) | 6 (33%) | 4 (22%) | .296 |
| Deceased within the first year after radical cystectomy n(%) | 10 (11) | 5 (62%) | 1 (12%) | 2 (25%) | .718 |
Physical activity levels
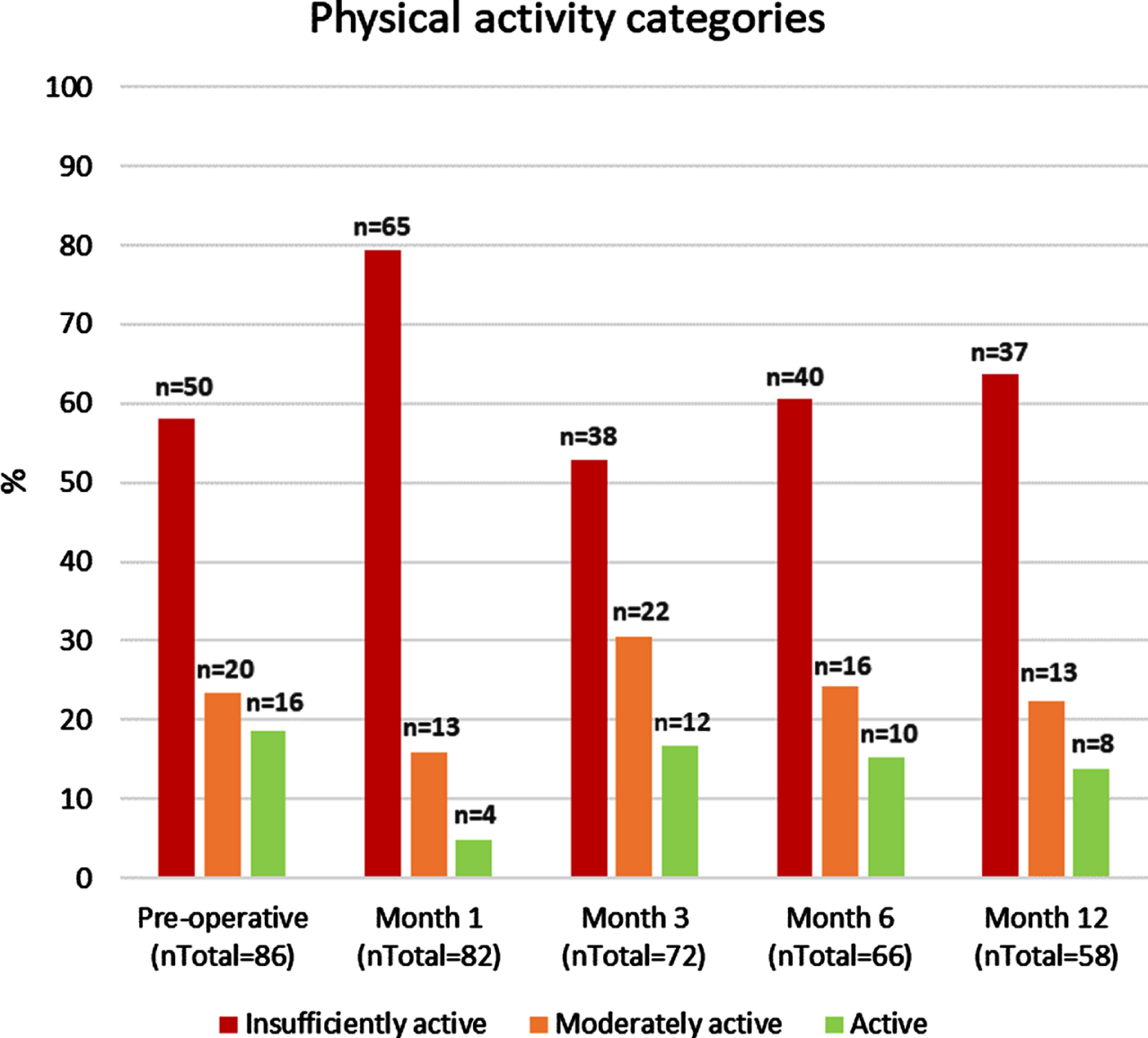
At each time point, the majority of BC patients (>50%) were insufficiently active (Fig. 1). Among patients in the moderately active or active group, light-intensity activities (mainly walking) were important contributors to the total amount of PA. Preoperatively, 16 of 36 (44%) patients in the moderately active and active group reported only light-intensity activities. Postoperatively, 16 of 17 (94%), 23 of 34 (68%), 17 of 26 (65%), 8 of 21 (38%) of patients in the moderately active or active group reported only light-intensity activities at month one, three, six and twelve, respectively.
Fig. 1
Physical activity categories according to the Godin Leisure Time Questionnaire from baseline to one year after radical cystectomy.
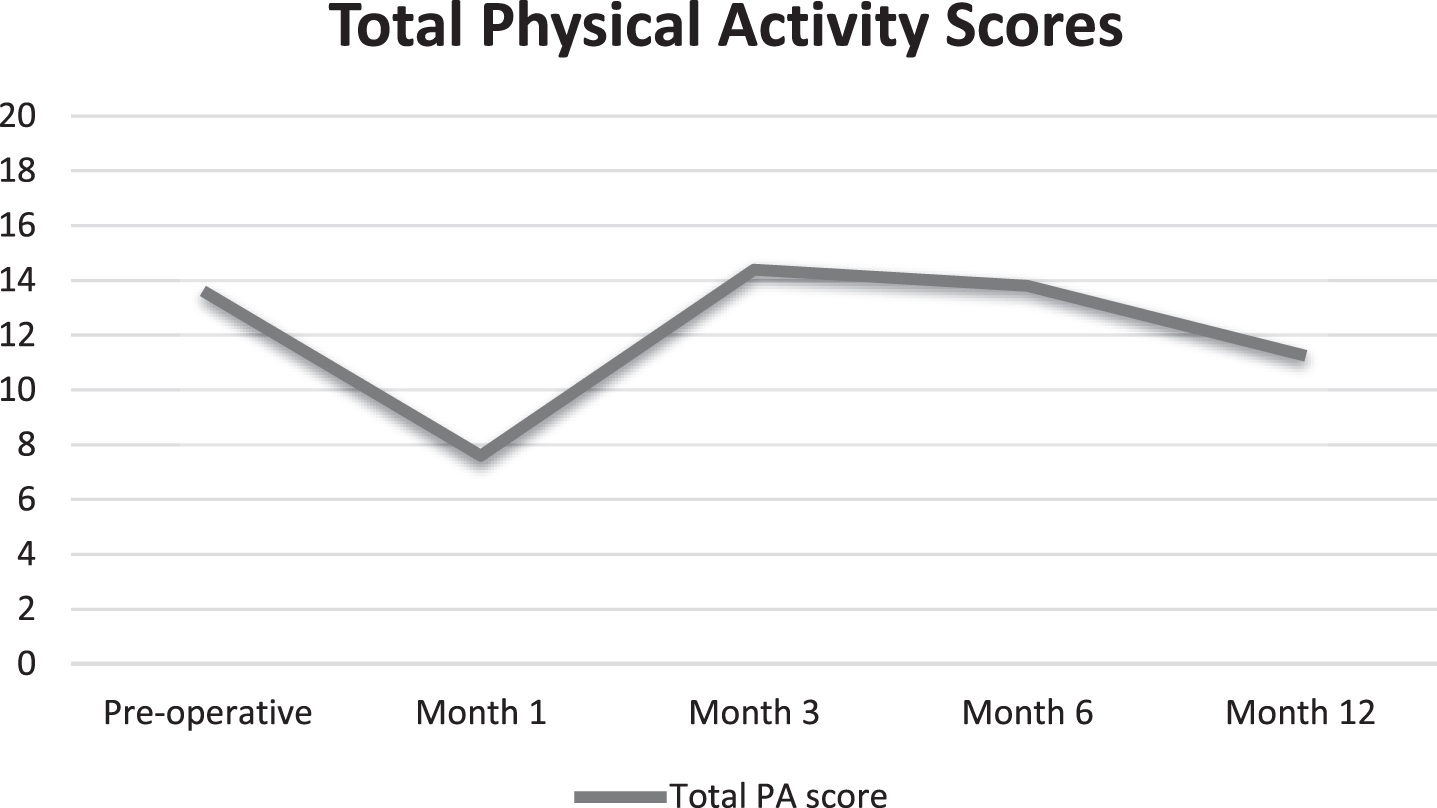
Overall, a significant change over time was seen for the total PA scores (p < 0.001) with significantly lower PA levels at month one compared to all other time-points (baseline, -5.9; month 3, -6.8; month 6, -6.2; month 12, -3.4). No significant differences were seen between the other time-points, indicating that PA levels were more or less the same at baseline, month three, six and twelve. Figure 2 presents a visual overview of the change in total PA scores over time.
Fig. 2
Total Physical activity scores over time (p < .001).
Health-related quality of life and comparisons with thresholds for clinical importance
Means and 95% confidence intervals for the HRQoL domains are presented in Table 2. Overall, significant changes over time were seen for all HRQoL domains except for cognitive functioning (p = 0.561) and bowel symptoms (p = 0.064). In general, the HRQoL outcomes were worst one month after RC.
Table 2
HRQoL outcomes (Estimated mean [95% CI]) over time compared to thresholds for clinical importance
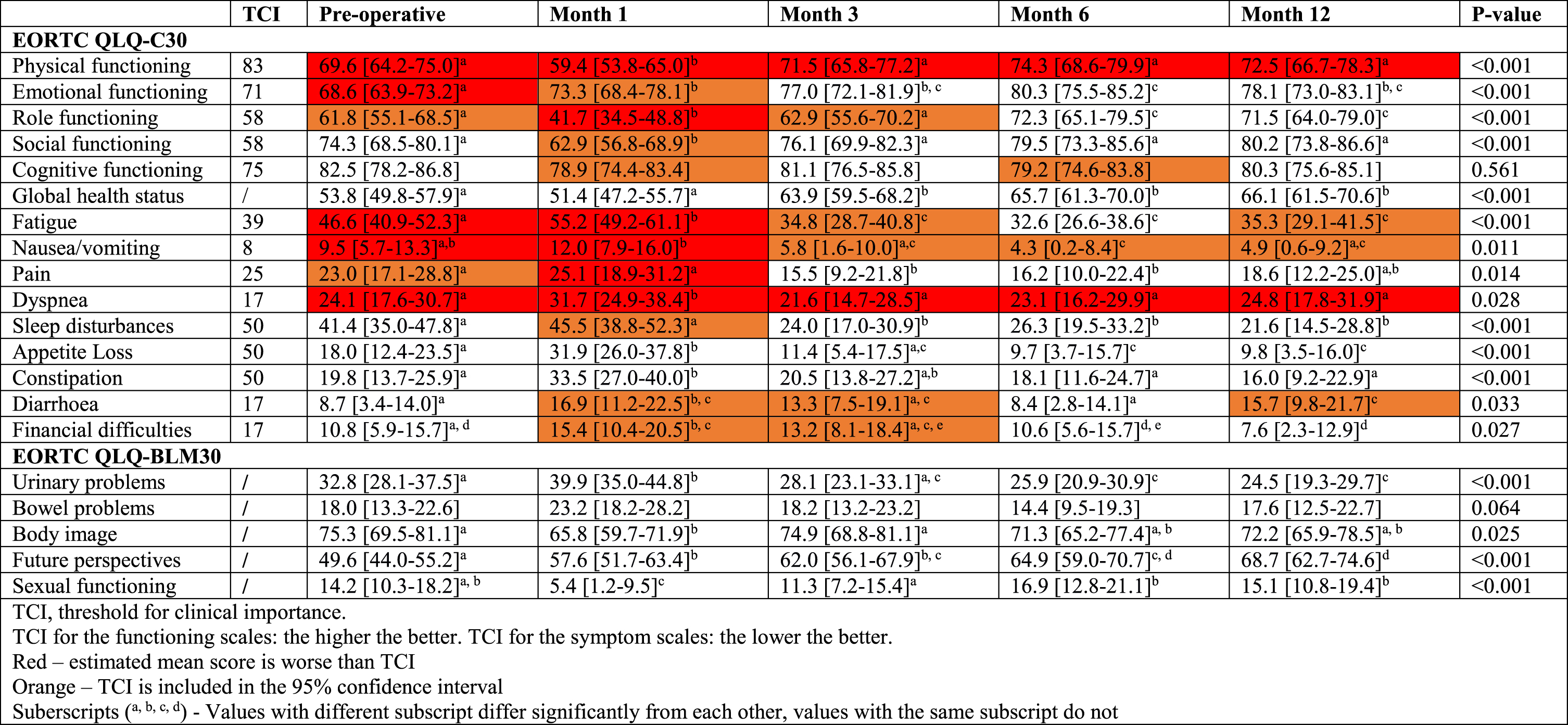 |
Comparisons of cancer-specific HRQoL domains with published thresholds for clinical importance (TCI) showed that physical functioning and dyspnoea scored worse than the thresholds at all time-points (i.e. TCI not in 95% confidence interval). Fatigue and nausea/vomiting scored worse than the thresholds at baseline and month one. Emotional functioning scored worse at baseline, whereas role functioning and pain scored worse at month one.
Associations between demographic, clinical and behavioural factors and physical activity
Univariate analysis showed that health literacy at baseline was the only significant predictor of PA across time-points (p = 0.003). Patients with lower health literacy levels reported higher PA levels compared to patients with higher health literacy levels.
Preoperative PA and HRQoL at month one and three
After adjusting for age and health literacy, patients in the active group before RC had significantly better outcomes one month after RC for physical functioning (mean difference (MD) -22.7, standard error (SE) 8.7, p = 0.011), fatigue (MD 19.9, SE 9.5, p = 0.038), and global health status (MD -15.9, SE 6.9, p = 0.023) compared to inactive patients. Also, active patients before RC had significantly better outcomes one month after RC for global health status (MD -18.6, SE 7.7, p = 0.017) compared to moderately active patients. Patients in the moderately active group before RC showed significantly more sleep disturbances (MD -22.8, SE 7.8, p = 0.004) at month one compared to inactive patients. No other significant differences were found at month one and three. Table 3a shows estimated mean scores and 95% confidence intervals of the HRQoL outcomes for each PA category.
Table 3a
Comparisons of HRQoL according to preoperative PA levels (estimated means [95% CI]; n = 85)
| Month 1 | Month 3 | |||||
| Inactive | Moderately active | Active | Inactive | Moderately active | Active | |
| Physical functioning | 55.8 [47.7-63.9] | 59.9 [48.3-71.5] | 78.5 [62.9-94.1]* | 70.3 [61.9-78.7] | 76.2 [64.4-87.9] | 74.1 [59.3-88.9] |
| Emotional functioning | 70.1 [62.9-77.2] | 67.3 [57.0-77.5] | 80.9 [67.0-94.9] | 72.7 [65.3-80.1] | 76.1 [65.7-86.4] | 78.2 [65.1-91.3] |
| Global | 48.8 [42.7-54.9] | 46.2 [37.3-55.1] | 64.8 [52.3-77.3]*° | 64.8 [58.4-71.3] | 57.8 [48.7-66.9] | 64.0 [52.5-75.5] |
| Fatigue | 61.8 [53.2-70.4] | 52.1 [39.6-64.4] | 41.9 [24.9-58.9]* | 34.7 [25.7-43.6] | 37.2 [24.6-47.8] | 31.3 [15.4-47.2] |
| Sleep disturbances | 39.5 [30.5-48.4] | 62.3 [49.1-75.4]** | 43.2 [24.4-62.0] | 24.4 [14.9-33.9] | 25.7 [12.2-39.2] | 25.2 [8.2-42.3] |
| Sexual functioning | 4.9 [-0.73-10.5] | 13.8 [5.6-22.2] | 13.6 [2.6-24.1] | 12.1 [6.2-17.9] | 18.3 [10.3-26.3] | 19.3 [9.3-29.2] |
*p<0.05, **p<0.01, ***p<0.001 (compared with inactive patients). °p<0.05, °°p<0.01, °°°p<0.001 (compared with moderately active patients).
Postoperative PA at month three and HRQoL at month six and twelve
After adjusting for age and health literacy, patients in the moderately active group at month three had significantly better physical functioning (MD -16.2, SE 6.9, p = 0.023) at month twelve compared to inactive patients. Moderately active patients at month three had significantly better sexual functioning levels at month six (MD -16.8, SE 5.4, p = 0.003) and twelve (MD -13.5, SE 5.5, p = 0.017) compared to inactive patients and at month six compared to active patients (MD 14.6, SE 7.2, p = 0.046). No other significant differences were found at month six and twelve. Table 3b shows estimated mean scores and 95% confidence intervals of the HRQoL outcomes for each PA category.
Table 3b
comparisons of HRQoL according to PA levels at month 3 after radical cystectomy (estimated means [95% CI]; n = 65)
| Month 6 | Month 12 | |||||
| Inactive | Moderately active | Active | Inactive | Moderately active | Active | |
| Physical functioning | 75.9 [66.5-85.2] | 87.4 [74.9-99.9]* | 78.4 [64.5-92.3] | 70.1 [60.5-79.6] | 86.3 [73.9-98.8] | 76.7 [62.9-90.7] |
| Emotional functioning | 76.8 [69.5-84.1] | 82.2 [72.5-91.9] | 82.6 [71.7-93.5] | 77.1 [69.5-84.7] | 79.6 [69.8-89.4] | 74.2 [63.3-85.2] |
| Global | 63.8 [56.5-71.1] | 67.7 [58.1-77.4] | 66.6 [55.7-77.5] | 63.3 [55.7-70.9] | 69.6 [59.8-79.4] | 65.8 [54.7-76.9] |
| Fatigue | 31.9 [22.1-41.9] | 27.7 [14.5-40.9] | 32.2 [7.4-47.0] | 38.1 [27.8-48.3] | 25.2 [12.0-38.4] | 41.5 [26.7-56.3] |
| Sleep disturbances | 22.4 [12.9-31.9] | 17.3 [4.6-29.9] | 23.2 [8.8-37.6] | 17.1 [6.9-27.3] | 17.3 [4.6-29.9] | 23.2 [8.8-37.6] |
| Sexual functioning | 15.9 [8.8-23.1] | 32.7 [23.0-42.5]** | 18.2 [7.8-28.5]° | 12.4 [4.8-19.9] | 25.9 [16.1-35.6]* | 23.7 [13.4-34.1] |
*p<0.05, **p<0.01, ***p<0.001 (compared with inactive patients).°p<0.05, °°p<0.01, °°°p<0.001 (compared with moderately active patients).
DISCUSSION
This study investigated PA patterns and HRQoL outcomes from diagnosis to one year after RC in BC patients and relationships between PA and HRQoL outcomes. This study shows that the majority of BC patients undergoing RC is inactive and have low HRQoL outcomes from diagnosis to one year after RC Furthermore, PA in the preoperative and postoperative time periods have positive associations with several HRQoL domains.
BC patients in the present study report already low PA levels at diagnosis which might be due to their older age and associated comorbidities as well as irritative urinary symptoms and multiple hospital visits which can be tiring [18]. In addition, the low HRQoL outcomes before RC might contribute to low PA levels (and vice versa). Postoperatively, treatment side-effects or adapting to a new urinary diversion can be tiring and consequently lead to lower PA levels [18]. Low PA levels among cancer patients are common and in line with published literature [19]. However, many studies in the literature did not include light-intensity activities [19]. In contrast, we have also taken into account light-intensity activities, causing less patients to be categorized as inactive.
Threshold for clinical importance were exceeded for physical functioning, dyspnoea, mental and role functioning, nausea/vomiting, pain and fatigue. These findings suggest that clinical attention is needed to prevent or manage one of these symptoms or domains of functioning. When measuring HRQoL in BC patients undergoing RC, it may be especially important to assess these symptoms which are clinical important and might require a clinical action.
In line with previous studies, BC patients have an impaired physical and mental HRQoL status already at time of diagnosis [1]. Mental functioning and future perspectives were especially low at diagnosis, but started to improve one month after RC. However, better reported emotional outcomes might not necessarily mean that there is a true improvement in emotional outcomes. A recent study found that most of the positive changes in emotional functioning were related to a reprioritization response shift [20]. Response shift is an important and emerging concept in the interpretation of HRQoL outcomes as the outcomes reported by patients might be influenced by adapting to new life situations and therefore prioritizing other things in life [21].
The physical HRQoL outcomes (e.g. fatigue, physical functioning) further decline from diagnosis to month one after RC and start to improve again from month three onwards. HRQoL outcomes three months after RC are already better than baseline HRQoL outcomes. However, returning to baseline HRQoL outcomes should not be the goal for BC patients since they already have low HRQoL outcomes at baseline. BC patients still report low physical HRQoL outcomes one year after RC which might be explained by the clinical recurrences of BC patients within the first year after RC (19 out of 90 patients in our cohort). A recent study [22] looked at HRQoL outcomes in BC survivors (1 to 10 years after RC) and found slightly better HRQoL outcomes (±5 points on the EORTC QLQ-C30 and BLM30 scales) [23] in their population compared to the HRQoL outcomes one year after RC in our population [22].
Also important to note is that our study sample consisted mainly of patients with an ileal conduit (71%). A previous study compared HRQoL outcomes between patients with an ileal conduit versus a neobladder and showed that patients with a neobladder have better physical functioning, role functioning, social functioning, global health status and financial expenditure compared to patients with an ileal conduit [24]. Findings from this previous study might help to explain the low HRQoL outcomes found in our study. However, the better HRQoL outcomes in patients with a neobladder compared to patients with an ileal conduit might also reflect the inherent younger and fitter patient population for this type of urinary diversion [25].
Interestingly, a few findings from this study were unexpected and need to be acknowledged. First, patients with lower health literacy levels reported significantly higher PA levels compared to patients with higher health literacy levels. This might be explained by the fact that self-reported PA data is less valid in a lower educated population [26]. If people with lower health literacy overestimate their PA levels, than the true PA levels are even lower than reported in this study. After adjusting for health literacy, however, PA remained a significant predictor of HRQoL. Secondly, more sleep disturbances were reported one month after RC in moderate active patients compared to inactive patients. Although age was not a significant predictor of PA in this study, we can only suggest that more younger people were part of the moderate active group compared to the inactive group and that younger people are more likely to receive a neobladder which might be responsible for more sleep disturbances (e.g. waking up at fixed time-points at night to empty neobladder). The last unexpected finding was that patients in the active group at month three after RC reported statistically worse sexual functioning at month six compared to moderate active patients. This finding might be contributed to the small sample size of this study which might have introduced a statistical type 1 error [27].
Implications for future research or clinical practice
Given the low PA levels and HRQoL outcomes, and the significant associations between PA and physical functioning, fatigue, global health status and sexual functioning, this study suggests the importance of further investigating the effects of PA interventions in BC patients.
First, PA interventions for BC patients should try to increase PA levels throughout their disease trajectory rather than returning to baseline (= diagnosis) PA levels. Second, a great proportion of BC patients engage in light-intensity activities which is also in line with a previous cross-sectional study concluding that BC patients prefer walking as PA type [28]. Including walking as an important component of future PA interventions might be a potential strategy to promote PA in BC patients. Previous walking interventions showed promising results to improve cancer patient outcomes [29].
Third, PA should not only be promoted in the postoperative period for BC patients. This study showed that both physical and mental HRQoL outcomes are already severely impaired before RC. Risk of morbidity and mortality following RC have been associated with preoperative risk factors such as functional status [30], nutritional deficiency [30] and mental health [31]. Therefore, the impaired physical and mental HRQoL status before RC highlights the importance of optimizing the preoperative status of BC patients. In order to further understand the effects of prehabilitation, future studies should investigate differences in effects on HRQoL between patients who were already active before diagnosis or started to become active in the prehabilitation trial.
Next to future interventional research, more efforts are needed to facilitate interpretation of HRQoL data in BC patients. First, thresholds for clinical importance for the EORTC QLQ-BLM30 would make it easier for clinicians and researchers to interpret BC specific HRQoL data [16]. Secondly, future investigations into the concept of response shift will inform researchers and clinicians on how to interpret improvements in HRQoL data in BC patients [21].
Limitations and strengths
An important limitation is the use of self-reported PA instead of objectively measured data with accelerometers which may have introduced recall bias, response shift, and social desirability bias [32]. Future research should use objective measures to investigate PA in BC patients. Furthermore, the sample size in this study is relative small and missing data increased over time (up to 35% at month 12). Small sample sizes could introduce type 2 errors whereby predictors or beneficial effects of PA could have been missed. In addition, small sample sizes could also introduce type 1 errors, meaning that statistically significant results could be false positive [27]. However, in addition to the significant findings in our study, the results for the same variables also showed clinically important differences between the physical activity groups (>10 points difference on the EORTC QLQ-C30 scales) [23]. Given the low sample size in this study, differences in PA and HRQoL between type of urinary diversion were not investigated. Future studies with larger sample sizes should investigate this further. This was a multicentric study, enhancing the external validity of the study results. However, as only 2 centres were involved from a single country, our results should be replicated in other BC populations, places, and time periods.
To our knowledge, this is the first longitudinal study in BC patients investigating PA and HRQoL outcomes from diagnosis to one year after RC. The results of this study can guide the design of future PA interventions in BC patients as well as the rationale to develop other supportive care interventions to improve specific HRQoL outcomes at certain time-points. The use of thresholds for clinical importance was furthermore of added value to the interpretation of our study results.
Conclusion
This study showed that the majority of BC patients undergoing RC is inactive and have low HRQoL outcomes from diagnosis to one year after RC with the lowest scores at time of diagnosis and one month after RC. This study also showed benefits of PA for HRQoL outcomes in both the preoperative and the postoperative period. The data suggests that PA interventions could be an asset to improve BC patients’ HRQoL, but should be tested in future trials.
ACKNOWLEDGMENTS
This study was supported by ‘Kom Op Tegen Kanker’. JVC was supported by a Postdoctoral Fellowship of the Research Foundation Flanders (FWO, 12I1117 N).
AUTHOR CONTRIBUTIONS
Conception: ER, AVH, SV, VF
Performance of work: ER, KD, MA
Interpretation of data: ER, RC, AVH, VF, JVC, BR
Writing the article: ER, AVH, JVC, KD, LP, RB, MA, SV, MVH, BD, VF
CONFLICT OF INTEREST
No conflict of interest to report by ER, AVH, JVC, KD, LP, BR, RB, MA, SV, MVH, RC, BD, and VF.
REFERENCES
[1] | Mohamed NE , Herrera PC , Hudson S , Revenson TA , Lee CT , Quale DZ , et al., Muscle invasive bladder cancer: examining survivor burden and unmet needs, The Journal of Urology (2014) ;191: (1):48–53. |
[2] | Mohamed N , Diefenbach M , Goltz H , Lee C , Latini D , Kowalkowski M , et al. Muscle invasive bladder cancer: from diagnosis to survivorship. Advances in Urology. 2012. |
[3] | Clements MB , Atkinson TM , Dalbagni GM , Li Y , Vickers AJ , Herr HW , et al. Health-related Quality of Life for Patients Undergoing Radical Cystectomy: Results of a Large Prospective Cohort. European Urology. 2021. |
[4] | Catto JWF , Gordon K , Collinson M , Poad H , Twiddy M , Johnson M , et al. Radical Cystectomy Against Intravesical BCG for High-Risk High-Grade Nonmuscle Invasive Bladder Cancer: Results From the Randomized Controlled BRAVO-Feasibility Study, J Clin Oncol (2021) ;39: (3):202–14. |
[5] | Shariat SF , Milowsky M , Droller MJ , Bladder cancer in the elderly. Urologic Oncology: Seminars and Original Investigations; (2009) : Elsevier. |
[6] | Winters B , Schade G , Holt S , Gore J , Dash A , Porter M , et al. MP72-19 the impact of health related quality of life on cystectomy patients using the medical health outcomes study, The Journal of Urology (2015) ;193: (4S):e928–e. |
[7] | Buffart LM , Kalter J , Sweegers MG , Courneya KS , Newton RU , Aaronson NK , et al. Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treatment Reviews. 2016.3;. |
[8] | Hijazi Y , Gondal U , Aziz O . A systematic review of prehabilitation programs in abdominal cancer surgery. International Journal of Surgery. 2017. |
[9] | Rammant E , Decaestecker K , Bultijnck R , Sundahl N , Ost P , Pauwels NS , et al. A systematic review of exercise and psychosocial rehabilitation interventions to improve health-related outcomes in patients with bladder cancer undergoing radical cystectomy. Clinical Rehabilitation. 2017:0269215517746472. |
[10] | Kaye DR , Schafer C , Thelen-Perry S , Parker C , Iglay-Reger H , Daignault-Newton S , et al. The Feasibility and Impact of a Presurgical Exercise Intervention Program (Prehabilitation) for Patients Undergoing Cystectomy for Bladder Cancer, Urology (2020) ;145: :106–12. |
[11] | Campbell KL , Winters-Stone KM , Wiskemann J , May AM , Schwartz AL , Courneya KS , et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable (2019) ;51: (11):2375–90. |
[12] | Amagasa S , Machida M , Fukushima N , Kikuchi H , Takamiya T , Odagiri Y , et al. Is objectively measured light-intensity physical activity associated with health outcomes after adjustment for moderate-to-vigorous physical activity in adults? A systematic review, International Journal of Behavioral Nutrition and Physical Activity. (2018) ;15: (1):65. |
[13] | Blair CK , Morey MC , Desmond RA , Cohen HJ , Sloane R , Snyder DC , et al. Light-intensity activity attenuates functional decline in older cancer survivors, Med Sci Sports Exerc (2014) ;46: (7):1375–83. |
[14] | Godin G . The Godin-Shephard Leisure-Time Physical Activity Questionnaire, The Health & Fitness Journal of Canada (2011) ;4: (1):18–22. |
[15] | Aaronson NK , Ahmedzai S , Bergman B , Bullinger M , Cull A , Duez NJ , et al. The European Organization for Research and Treatment of Cancer QLQ-C a quality-of-life instrument for use in international clinical trials in oncology, JNCI: Journal of the National Cancer Institute (1993) ;85: (5):365–76. |
[16] | Giesinger JM , Loth FL , Aaronson NK , Arraras JI , Caocci G , Efficace F , et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research, Journal of clinical epidemiology (2020) ;118: :1–8. |
[17] | Schrack JA , Gresham G , Wanigatunga AA . Understanding physical activity in cancer patients and survivors: new methodology, new challenges, and new opportunities, Cold Spring Harb Mol Case Stud (2017) ;3: (4):a001933. |
[18] | Rammant E , Fonteyne V , Decaestecker K , Bultijnck R , Deforche B , Pieters R , et al. Understanding physical activity behavior in patients with bladder cancer before and after radical cystectomy: a qualitative interview study, Clinical Rehabilitation (2019) ;33: (4):750–61. |
[19] | Rammant E , Bultijnck R , Caperchione CM , Trinh L , editors, The Use of Theory to Develop Physical Activity Interventions in Urological Cancer Survivors: A Narrative Review. Seminars in Oncology Nursing; 2021: Elsevier. |
[20] | Murata T , Suzukamo Y , Shiroiwa T , Taira N , Shimozuma K , Ohashi Y , et al. Response Shift–Adjusted Treatment Effect on Health-Related Quality of Life in a Randomized Controlled Trial of Taxane Versus S-1 for Metastatic Breast Cancer: Structural Equation Modeling, Value in Health (2020) ;23: (6):768–74. |
[21] | Ilie G , Bradfield J , Moodie L , Lawen T , Ilie A , Lawen Z , et al. The role of response-shift in studies assessing quality of life outcomes among Cancer patients: a systematic review, Front Oncol (2019) ;9: :783. |
[22] | Catto JW , Downing A , Mason S , Wright P , Absolom K , Bottomley S , et al. Quality of life after bladder cancer: A cross-sectional survey of patient-reported outcomes, European Urology (2021) ;79: (5):621–32. |
[23] | Cocks K , King M , Velikova G , De Castro G , St-James MM , Fayers P , et al. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30, European Journal of Cancer (2012) ;48: (11):1713–21. |
[24] | Singh V , Yadav R , Sinha RJ , Gupta DK . Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model, BJU Int (2014) ;113: (5):726–32. |
[25] | Rammant E , Van Wilder L , Van Hemelrijck M , Pauwels NS , Decaestecker K , Van Praet C , et al. Health-related quality of life overview after different curative treatment options in muscle-invasive bladder cancer: an umbrella review, Quality of Life Research (2020) ;29: :2887–910. |
[26] | Winckers ANE , Mackenbach JD , Compernolle S , Nicolaou M , van der Ploeg HP , De Bourdeaudhuij I , et al. Educational differences in the validity of self-reported physical activity, BMC Public Health (2015) ;15: :1299. |
[27] | Christley R . Power and error: increased risk of false positive results in underpowered studies, The Open Epidemiology Journal (2010) ;3: (1). |
[28] | Karvinen KH , Courneya KS , Venner P , North S . Exercise programming and counseling preferences in bladder cancer survivors: a population-based study, Journal of Cancer Survivorship: Research and Practice (2007) ;1: (1):27–34. |
[29] | Frensham LJ , Parfitt G , Dollman J . Effect of a 12-Week Online Walking Intervention on Health and Quality of Life in Cancer Survivors: A Quasi-Randomized Controlled Trial, International Journal of Environmental Research and Public Health (2018) ;15: (10):2081. |
[30] | Lyon TD , Farber NJ , Chen LC , Fuller TW , Davies BJ , Gingrich JR , et al. Total psoas area predicts complications following radical cystectomy. Advances in Urology. 2015;2015. |
[31] | Sharma P , Henriksen CH , Zargar-Shoshtari K , Xin R , Poch MA , Pow-Sang JM , et al. Preoperative patient reported mental health is associated with high grade complications after radical cystectomy, The Journal of Urology (2016) ;195: (1):47–52. |
[32] | Douma JAJ , de Beaufort MB , Kampshoff CS , Persoon S , Vermaire JA , Chinapaw MJ , et al. Physical activity in patients with cancer: self-report versus accelerometer assessments, Supportive Care in Cancer (2020) ;28: (8):3701–9. |




