Challenging Cases in Urothelial Cancer
Case 7 UR
Introduction
Approximately 80 per cent of patients who have a urothelial tumor of the bladder have a low or high grade papillary tumor which is non invasive (Ta) or is high grade papillary or sessile and invades the lamina propria (T1). The initial presentation is most commonly gross hematuria, which promptly leads to outpatient endoscopy and a subsequent transurethral resection (TUR BT). The goal is complete endoscopic removal of all visible tumors. This can be accomplished a variety of ways depending on the perceived depth of involvement or stage. One can use a cold cup instrument with subsequent cauterization, monopolar or bipolar loop resection, and adjunctive blue light or narrow band imaging (NBI) to aid white light endoscopy. Despite the goal of a complete resection there is a high chance of a subsequent tumor event; commonly termed a recurrence. There are several reasons for this: 1. Incomplete resection, 2. Missed tumor, 3. Tumor implantation on the altered urothelial surface, and 4. The continued effect of carcinogens on the urothelium. The urologist has an important role in minimizing the chance of a “recurrence”. This includes diligence in performing a “complete” initial resection, use of blue light or NBI if available, consideration of postoperative intravesical chemotherapy (POIVC), and emphasis on smoking cessation.
The following case is a common one and suggests one of the options for removing tumors in an elderly patient with recurrent Ta bladder tumors. We invite our readers to review and comment on the case and management by using the online comment section below the case: https://www.bladdercancerjournal.com/challenging-cases.
Case
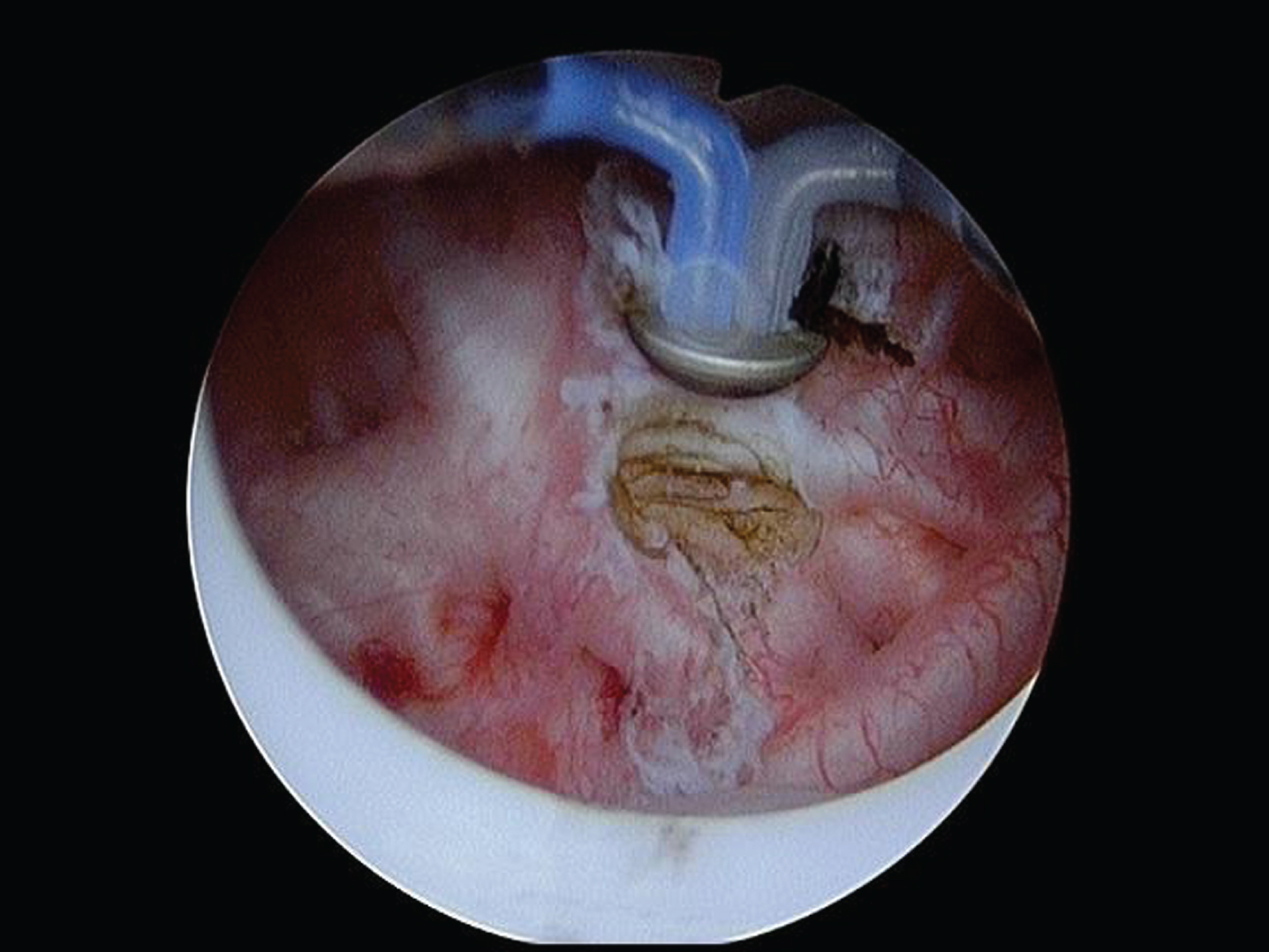
Fig.1
2–3 cm papillary tumors posterior wall.

Fig.2
Cold cup biopsy forceps to remove a tumor.

Fig.3
The button is used to cauterize remaining tumor and base of removed tumors.
The patient is a 95 year old man with multiple medical problems, which include chronic obstructive pulmonary disease and mitral regurgitation. Despite his age and co morbid diseases he lives independently. He has few voiding complaints other than nocturia.
Fig.4
Tumors all removed with the cold cup biopsy forceps.

He has a several year history of grade 2 and 3 Ta papillary tumors. His most recent TUR BTs were Sept. 2015, September 2016, August 2017, and November 2017. He had one six-week course of BCG followed by maintenance in 2016 after resection of mostly grade 3 Ta tumors. In March 2018 I performed the most recent office flexible endoscopy, which revealed multiple papillary low grade (1-2) appearing Ta tumors.
The patient was taken to the operating room for a TUR BT. Prior to the procedure I had my customary consultation with the anesthesiologist as a part of my preoperative check list and requested that the patient be paralyzed either with general endotracheal tube anesthesia or a spinal anesthetic. It is most important that the patient remain still during the procedure. Perforation during a TUR BT should be a rarity as long as the urologist has proper equipment, controls the bladder volume, i.e. keep the bladder at half volume during the resection, and does not have to contend with bladder motion.
In this case I elected, as I commonly do, to use the cold cup biopsy forceps to remove most of thepapillary tumors. This provides a nice specimen devoid of cautery for the pathologist and minimizes the risk of creating a deeper opening in the bladder than necessary. This is a patient who has never had an invasive tumor and has had multiple prior resections. Once the majority of the tumors were removed I used the bipolar button to cauterize the base of the resected tumors and vaporize remaining small papillary tumors. I used the bipolar resectoscope since the patient had a pacemaker. I used both white light and NBI during and after the procedure to help ensure a complete resection. I always begin and conclude each TUR BT with a survey of the bladder with a 70-degree lens. I use either a 12 or 30-degree lens during the TUR BT depending on the tumor location.
The pathology report indicated the tumors were low grade (grade 2) Ta.
Questions:
1. Do you use a check list prior to a TUR BT?
2. What type of anesthesia do you prefer?
3. Do you prefer monopolar or bipolar resection?
4. Do you utilize blue light or NBI and when?
5. Do you use the cold cup to remove bladder tumors?
6. When do you give postoperative intravesical chemotherapy?
Case 8 NF
Introduction
Low-grade bladder tumors are almost always confined to the urothelial surface. They are arguably the most common urothelial tumor in the urinary tract. The current grading system uses low and high grade instead of the now historical 1–3 grading system. Low-grade tumors include not only those that were previously called grade 1 but also some of the grade 2 tumors. If the pathologist believes there is “significant” atypia they will classify the bladder cancer as high grade. Thus high grade incorporates not only all the prior grade 3 but also many of the prior grade 2 tumors. In an analysis of a 10 year span of pathology reports from The University of Miami we demonstrated a significant decline in reports of low grade bladder cancer with a corresponding increase in those called high grade. In other words there has been a grade migration. This is important as it may lead to overtreatment for some patients.
Fig.5
Papillary bladder tumors.
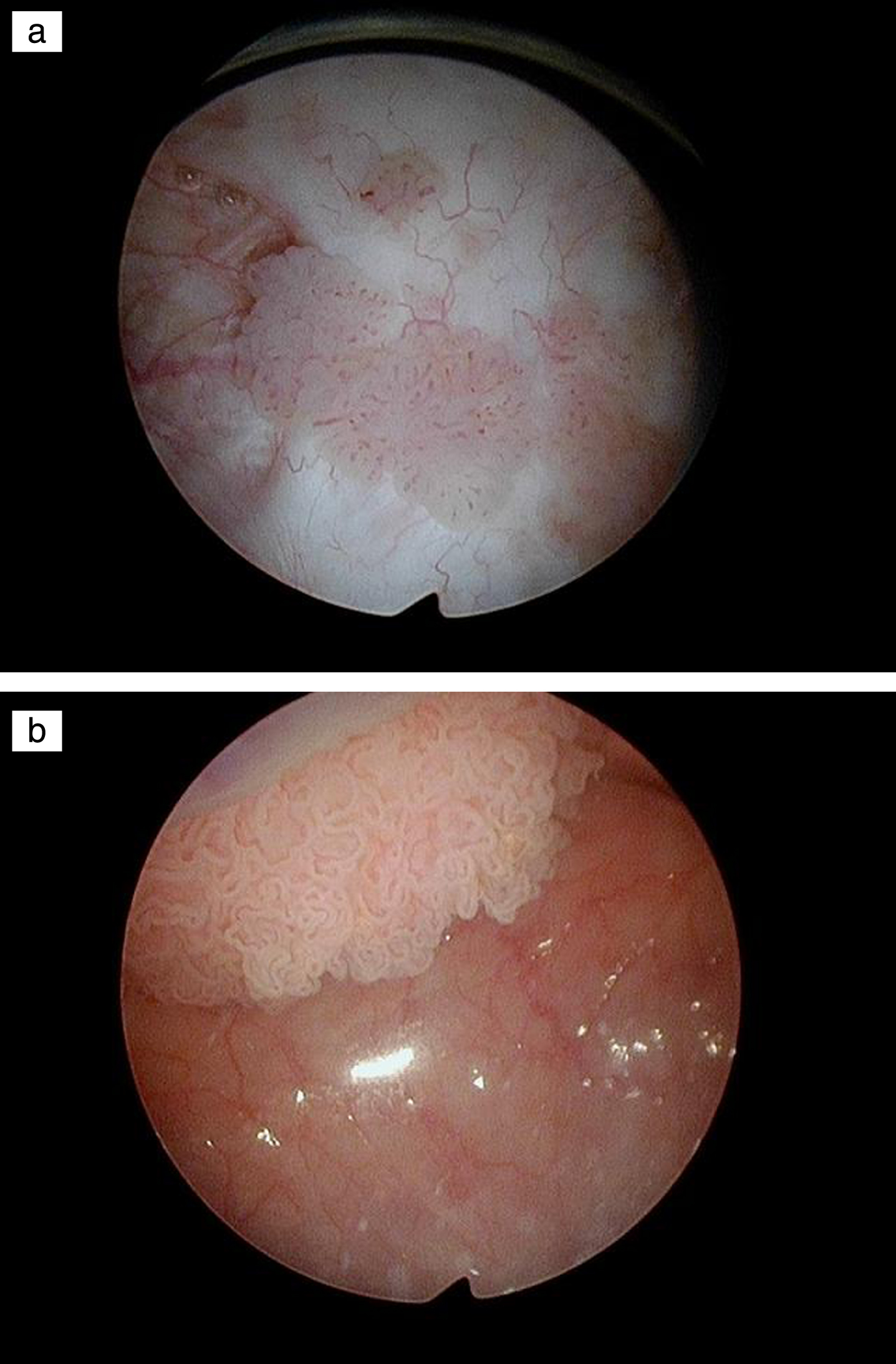
The current EAU and SUO/AUA guidelines state that patients with low risk bladder tumors have a single initial papillary low grade tumor less than 3 cm. Any case of primary multifocal low grade Ta bladder cancer or any patient with “recurrent” low or high grade Ta tumor regardless of size are in the intermediate risk category. If we believe the risk category should classify patients according their risk of progression then all patients with low-grade tumors should be low risk since they rarely develop an invasive bladder cancer. They may be at intermediate risk for a “recurrence” if they have multifocal or large tumors but they are at very low risk of progression, which, in my view, is the most important prognostic factor in determining treatment decisions.
Fig.6
Papillary tumor in the prostatic urethra.
Urothelial cancer in the prostatic urethra is relatively uncommon. Grade and depth of invasion are critical as it relates to the extent of resection and consideration of subsequent treatment. The current case involves a man with low-grade non invasive appearing tumor in the prostatic urethra in addition to tumors in the bladder. We invite our readers to review and comment on the case and management by using the online comment section below the case: https://www.bladdercancerjournal.com/challenging-cases.
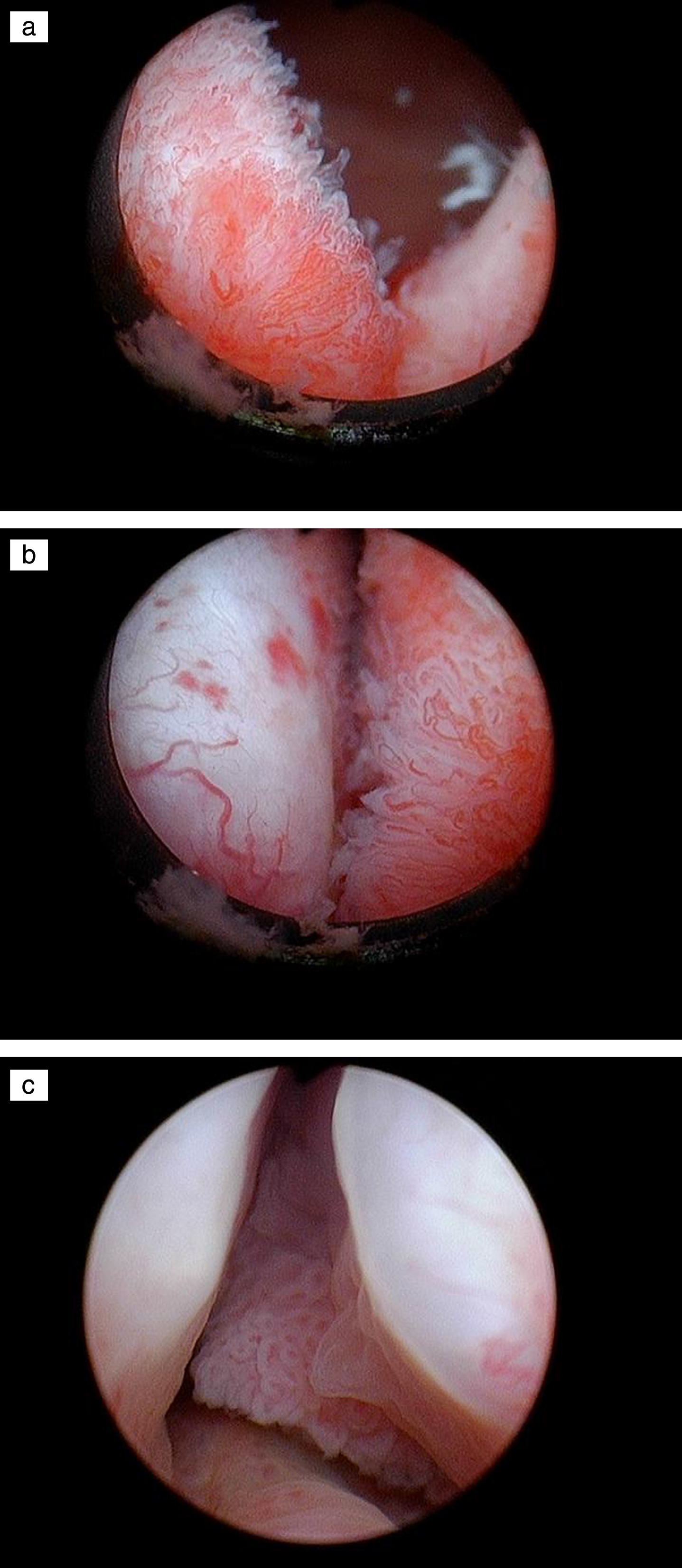
Case
This is a 70 year old man with a heavy cigarette smoking history and despite stopping at age 50 he has moderately severe chronic obstructive pulmonary disease (COPD) as well as a history of recurrent low and high-grade non invasive (Ta) bladder cancer. The most recent outpatient flexible cystoscopy identified several papillary Ta appearing tumors in the bladder and similar tumors on the surface of the prostatic urethra.
He has minimal lower urinary tract symptoms (LUTS). He gets up once at night to void and does not have daytime frequency. His post void residual urine is 32 ml.
He has undergone a formal transurethral resection of bladder tumors (TUR BT) approximately every two years over the past decade. In addition to formal TUR BTs I have cauterized small papillary low-grade Ta appearing tumors in the office on several occasions. During the most recent office cystoscopy I observed several small and medium size bladder tumors and also papillary low grade appearing tumor in the prostatic urethra.
In the preoperative holding area prior to surgery I reviewed my checklist and as an important part of that I discussed the case with the attending anesthesiologist. He told me that the patient was having an acute exacerbation of bronchitis and he did not feel a general anesthetic was appropriate however the patient agreed to a spinal anesthetic. I consented the patient for a TUR BT as well as a transurethral resection of the prostate (TURP).
I realize there are several alternatives for eradicating the apparent “superficial” tumor in the prostatic urethra (PU). This includes a formal TURP, laser or roller ball cauterization, or cold cup biopsy followed by cautery.
I began the procedure by inserting a continuous flow resectoscope using a visual dilator. I used a 70 lens to review the entire bladder and confirmed the presence of several papillary bladder tumors. They ranged from 1–3 cm and were located on the posterior and anterior walls. The papillary tumor in the PU was present at the bladder neck/median lobe of the prostate, along sections of both lateral walls and near the verumontanem.
I removed the bladder tumors by a standard TUR BT using the monopolar resectoscope. Given the current appearance of the tumors and his history of only having Ta tumors I made no attempt to resect beyond the lamina propria. I proceeded to perform a limited TURP. I felt confident that the tumors were low grade and almost certainly noninvasive. Following the procedure a catheter was placed and the patient was discharged home and instructed to remove the catheter in 2 days.
Would you have proceeded in a different fashion?
Would you give him postoperative intravesical chemotherapy?



