Challenging Cases in Urothelial Cancer
INTRODUCTION
Urothelial cancer of the urinary tract is common and affects a large number of men and women, resulting in a reasonably large part of the work effort of urologists who take care of adults. Most of the urothelial tumors arise in the bladder but the same causative factors can lead to similar tumors in the kidneys, ureters, prostate, and urethra. Due to the heterogeneous nature of these tumors as well as their propensity for “recurring” in time and location over the patient’s life the clinician is often in the position of deciding among often challenging treatment choices for his/her patient. Although there are published guidelines many cases do not readily fit into a typical scenario, thus leaving ample room for decision making for the individual patient. We invite our readers to review and comment on the case and management by using the online comment section below each case: https://www.bladdercancerjournal.com/challenging-cases
Case 6
R.F. is a healthy appearing 55 year old man who had gross hematuria February 2016. His past medical history is negative with the exception of a 15 pack/year history of cigarette smoking. He had a normal CT scan with the exception of a bladder tumor located in the posterior wall of the bladder. He underwent an uneventful transurethral resection of a papillary bladder tumor in March 2016 at another medical center.
He received a single postoperative dose of intravesical mitomycin C 40 mg in 40 ml in the recovery room.
The pathology report indicated a high grade (grade 3) urothelial carcinoma which invaded the lamina propria. There was muscularis propria present in the specimen and there was no invasion beyond the lamina propria.
The patient did not receive additional adjuvant therapy. He began to have marked urinary frequency and dysuria shortly after the TUR BT.
I initially saw him in December 2016. He still had marked lower urinary tract symptoms. He voids every 1–2 hours – day and night. Anticholinergic medications were tried without improvement. He has not had a urinary tract infection.
A flexible cystoscopy in December 2016 revealed a 4–5 cm denuded area on the posterior wall of the bladder with calcifications on the surface. There was no obvious tumor in the bladder. A voided and bladder wash urine for cytology indicated atypical cells.
Although an office cystoscopy in March 2017 was unchanged a urine cytology was reported as high grade urothelial cancer. Cystoscopy and bladder biopsies were therefore performed under anesthesia. The same denuded area was observed on the posterior wall. The rest of the bladder appeared normal as did the prostatic urethra. Cold cup bladder biopsies did not indicate cancer. Urine cytology was again consistent with high grade cancer.
I performed a flexible cystoscopy and obtained urine for cytology in October 2017. The abnormal appearing concretions were again observed on the denuded urothelium on the posterior wall. The remainder of the bladder was normal. The cytology was again positive for high grade cancer.
The patient’s voiding symptoms persist and are a major quality of life problem.
A recent CT scan of the abdomen and pelvis is perfectly normal with the exception of a line of calcification at the posterior bladder wall consistent with the endoscopic findings.
What should one do? Possibilities include a partial cystectomy, total cystectomy or cystoprostatectomy and neobladder, or continued monitoring.
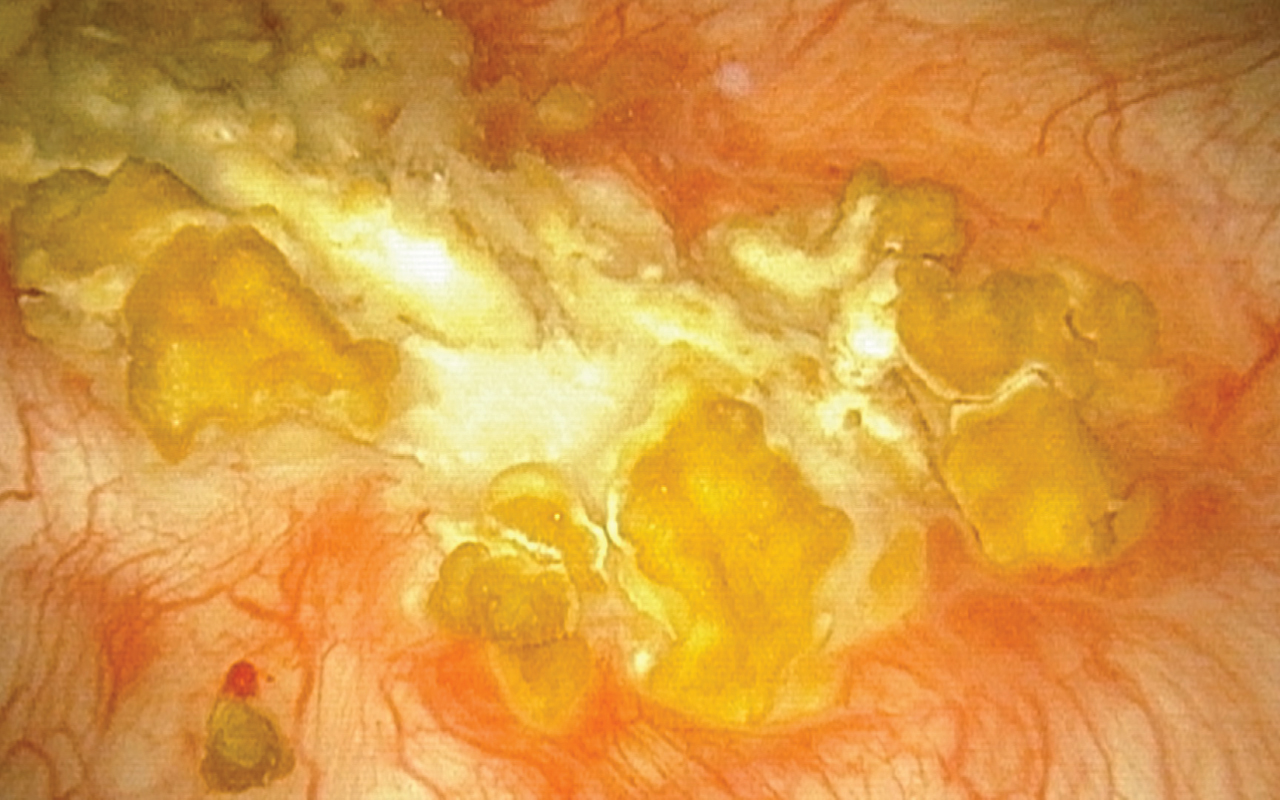
Photo.1
Endoscopic view of the calcified urothelium in March 2017.
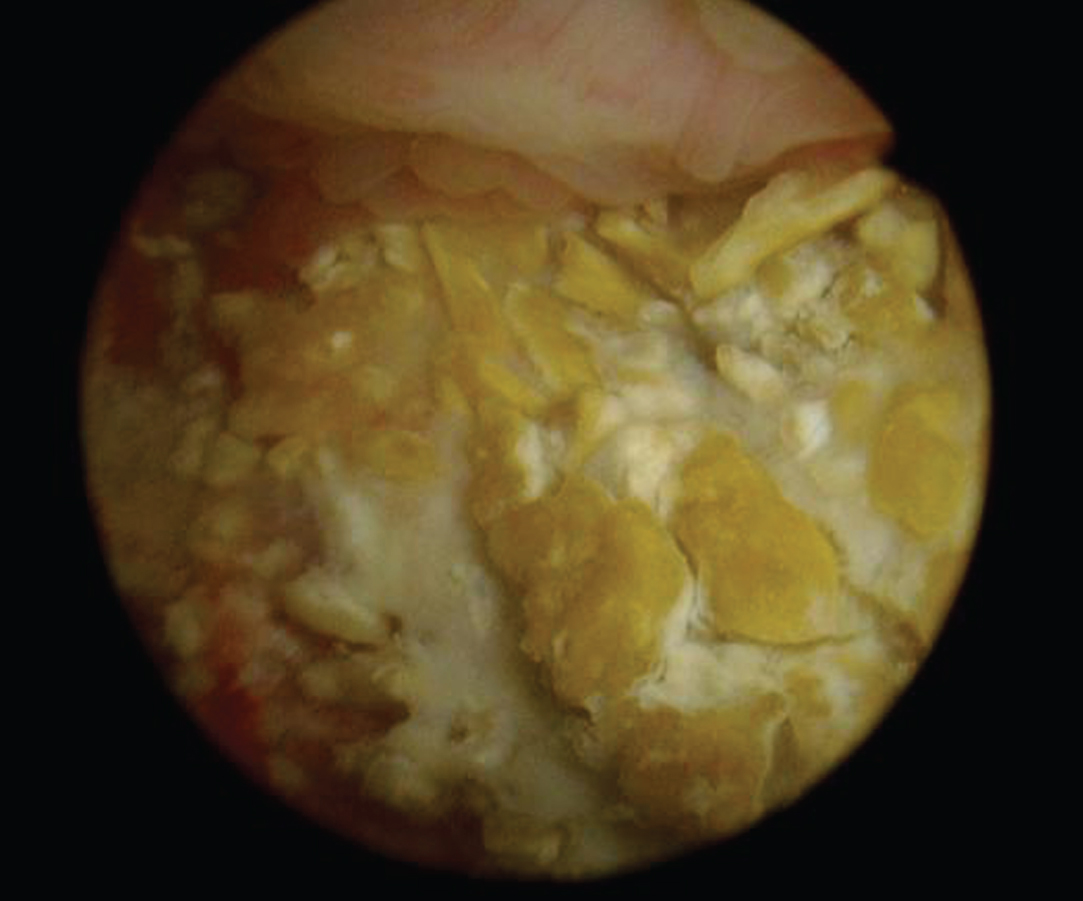
Photo.2
Office endoscopic photo of the calcified surface on the posterior wall of the bladder, Oct 2017.