Using Analytic Morphomics to Understand Short-Term Convalescence after Radical Cystectomy
Abstract
Background: Data from the general surgery literature suggests that patient morphometric data obtained from preoperative imaging may help predict a patient’s risk around surgery.
Objectives: In this context, we evaluated for associations between psoas muscle area and short-term convalescence following radical cystectomy.
Methods: After identifying patients who underwent radical cystectomy at our institution (2008 to 2013), we calculated their psoas muscle area from staging computed tomography scans using established analytic morphomic techniques. We then determined early recovery among patients with high and low psoas muscle area using the validated Convalescence and Recovery Evaluation (CARE) questionnaire—a 27-item survey, divided into four domains (activity, cognitive, gastrointestinal, and pain recovery). Finally, we assessed the relationship between psoas muscle area and changes in CARE scores with nested linear regression models.
Results: Among the 86 men and among 31 women in our cohort, the median total psoas muscle area was 2,544 mm2 and 1,511 mm2, respectively (P < 0.001 for the comparison). While there was no association between psoas muscle area and recovery in men, women with higher (versus lower) total psoas muscle area had smaller decreases in their pain scores postoperatively and a quicker return to their baseline level (P = 0.05). Activity scores also approached baseline levels faster among women with higher psoas muscle area, although this finding did not reach statistical significance.
Conclusions: Psoas muscle area is potentially an important preoperative predictor of recovery for women undergoingradical cystectomy. More broadly speaking, analytic morphomics may represent a novel approach to better understand perioperative risk.
INTRODUCTION
For patients with muscle invasive-bladder cancer, radical cystectomy is often considered first-linetreatment. This is a formidable operation, and evenin expert hands, it is associated with substantialperioperative morbidity and mortality [1]. Therefore, when selecting patients upon whom to operate, urologists must balance the indications for cystectomy with their perception of the patient’s ability to recover from it.
While several risk stratifications tools exist [e.g., the American Society of Anesthesiologists (ASA) Physical Status classification, Eastern Cooperative Oncology Group Scale of Performance Status], many are subjective in nature, leading to considerable inter-rater disagreement [2]. Moreover, they typically evaluate one portion of the patient’s operative risk [3, 4]. As such, much of a urologist’s clinical decision making relies on “clinical gestalt.” Thus, better objective measures of perioperative risk are needed. Emerging data from the general surgery literature suggests that patient morphometric characteristics gleaned from preoperative imaging (i.e., analytical morphomics) may fill this need [5, 6, 7, 8].
In this context, we performed a retrospective cohort study using data from our institution’s bladder cancer database. Among patients with muscle-invasive bladder cancer who underwent radical cystectomy, we assessed core muscle size from their preoperative staging computed tomography (CT) scans. We correlated these measures with patients’ postoperative convalescence assessed with a psychometrically robust questionnaire.
METHODS
Data sources and study population
For our study, we used a prospectively maintained bladder cancer database to identify all patients who underwent radical cystectomy at our institution between 2008 and 2013 (n = 1,623). A subset were consented to participate in a separate study, assessing patient-reported recovery after surgery (n = 154). The clinicopathological data from these patients were linked to their responses from a series of regularly timed pre- and postoperative questionnaires. Among this subset, 117 had their preoperative staging CT scans completed in our health system, which allowed us to make the morphometric measurements described below.
Exposure
Analytic morphomics refers to using cross-sectional imaging studies not only for the assessment of the specific pathology of interest, but also for a more global assessment of the patient. There is a growing body of literature, suggesting that morphometric data obtained from these studies can help predict surgical outcomes [5–12]. One of the more commonly used measurements is that of psoasmuscle area, which we calculated by identifying the cross-sectional area and density of the right and left psoas muscle at the level of the fourth lumbar vertebra. We also measured the average density (in Hounsfield Units) of the psoas muscle within these regions, which we then used to determine the total cross-sectional area excluding fatty infiltration (i.e., lean core muscle size). We completed these steps in a semi-automated fashion using previously established algorithms in MATLAB v 13.0 [5].
Outcomes
Our outcome of interest was patient-reportedearly recovery after radical cystectomy, assessed by the Convalescence And Recovery Evaluation (CARE) questionnaire [13]. The CARE questionnaire consists of 27 items that are divided into four quality of life (QoL) domains: activity, cognitive, gastrointestinal symptoms, and pain. The domain scores range from 0 to 100. Higher scores correspond to a better health state. The domain scores can be combined to generate a total score. Prior empirical work has shown that the CARE questionnaire has good internal consistency and test-retest reliability. Patients in our study completed the CARE questionnaire preoperatively and at 2, 4 and 6 weeks post-operatively.
Statistical analysis
First, we assessed our exposure variable—total psoas muscle area—for normality using descriptive statistics and histograms. We determined the median area for each gender. We used this value to dichotomize our population into groups of low versus high psoas muscle area.
Next, we made bivariate comparisons between patients with low versus high psoas muscle area, stratifying by gender. Specifically, we compared patients according to their QoL domains, their age at the time of surgery, race/ethnicity, ASA score, receipt of neoadjuvant chemotherapy, pathological stage, and urinary diversion type. We used both parametric and non-parametric tests as appropriate.
Finally, we evaluated the relationship between preoperative psoas muscle area and changes in CARE scores. To account for gender differencesand repeated measures, we fitted nested linearregression models. Our primary exposure was total psoas muscle area, nested within gender. We controlled for patient age and receipt of neoadjuvant chemotherapy. We performed our analyses using commercially available statistical software (SAS, version 9.1; SAS Institute, Inc.). All tests were two-tailed, and the probability of Type 1 error was set at 0.05. Our study had institutional review board approval.
RESULTS
Among the 86 men and among 31 women who underwent radical cystectomy at our institution between 2008 and 2013, the median total psoas muscle area was 2,544 mm2 and 1,511 mm2, respectively (Fig. 1, P < 0.001 for the comparison). For both men and women, patient demographic characteristics and disease severity measurements were similar between those with high and low psoas muscle area relative to the mean (Table 1, all P > 0.05). However, cross-sectional CT images taken at the level of the fourth lumbar vertebrae of two age-matched men from our cohort, one with high and the other low total psoas muscle area, show clear differences in morphometric measurements (Fig. 2).
After adjusting for age and neoadjuvant chemotherapy receipt, there was no association between psoas muscle area and recovery across any CARE QoL domains in men. However, women with higher total psoas muscle area had smaller decreases in their pain scores postoperatively and a quicker return to their baseline level (Fig. 3, P = 0.05). Activity scores also approached baseline levels faster among women with higher psoas muscle area, although this finding did not reach statistical significance. Our results persisted on sensitivity analyses where we examined the relationship between lean psoas muscle area and psoas muscle density and postoperative recovery in women, as well.
DISCUSSION
We found that core muscle size, as measured by total psoas muscle area, predicts pain recovery in women following radical cystectomy. These effects were independent of important preoperative patient characteristics, including age and receipt of neoadjuvant chemotherapy. In clearer terms, patients with low total psoas muscle area are not just older people with worse bladder cancer at baseline. Collectively, these findings suggest that analytic morphomics may be a useful and objective metric for understanding convalescence after radical cystectomy, at least among women.
Our study contributes to the growing body of literature on the utility of analytic morphomics in forecasting perioperative risk. Specifically, numerous studies have shown that quantitative measures of body composition can be used to predict morbidity and mortality among general surgical, vascular, and transplant patients [7, 9, 10, 11, 14]. While our findings were robust among women, no differencesin postoperative convalescence were observed between men with high versus low core muscle size. Similar gender-based findings have been shown with other morphomic measures, including abdominaladiposity. Mualla and colleagues found that visceral fat area predicted surgical complications among women but not men [15]. The reason for this observation is unclear, and it must be corroborated in follow-up studies.
Our study must be considered in the context of several limitations. First, our study was based on a relatively small sample of patients cared for at asingle hospital, and future work is necessary to validate our findings in broader populations. Second, given our study’s observational design, we cannot attribute causality between total psoas muscle area and postoperative convalescence in women. Third, there are numerous other morphometric measures that are captured on staging CT scans. While we focused on total psoas muscle area, we must acknowledge that these other measures may also serve as useful markers of perioperative risk.
Limitations notwithstanding, our data suggest that total psoas muscle area (and analytic morphomics more broadly) may serve as a useful objective risk stratification tool for women undergoing radical cystectomy. Urologists could use information that is routinely collected in the preoperative period to assess a patient’s fitness for surgery. For those patients deemed to be at high-risk for prolonged or complicated recovery, their provider could consider referral to a surgical health and optimization program to help prepare them for surgery.
CONCLUSIONS
In summary, our study suggests the possible benefit of morphomic data for predicting recovery in women undergoing radical cystectomy. Such information could potentially be used to help inform upfront clinical decision-making and counsel patients. Future prospective studies are needed to quantify the added value of analytic morphomics over other risk stratification tools.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
[1] | Boorjian SA , Kim SP , Tollefson MK , Carrasco A , Cheville JC , Thompson RH , Thapa P , Frank I . Comparative performance of comorbidity indices for estimating perioperative and 5-year all-cause mortality following radical cystectomy for bladder cancer. The Journal of Urology (2013) ;190: :55–60. |
[2] | Zimmerman C , Burman D , Bandukwala S , Seccareccia D , Kaya E , Bryson J , Rodin G , Lo C . Nurse and physician inter-rate agreement of three performance status measures in palliative care outpatients. Support Care Cancer (2010) ;18: :609–616. |
[3] | Fleisher LA , Eagle KA . Clinical Practice: Lowering cardiac risk in non-cardiac surgery. New England Journal of Medicine (2001) ;345: :1677–1682. |
[4] | Eagle KD , Berger PB , Calkins H , Chaitman BR , Ewy GA , Fleischmann KE , Fleisher LA , Froehlich JB , Gusberg RJ , Leppo JA , Ryan T , Schlant RC , Winters WL , Gibbons RJ , Antman EM , Alpert JS , Faxon DP , Fuster V , Gregoratos G , Jacobs AK , Hiratzka LF , Russell RO , Smith SC . ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery – executive summary. a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation (2002) ;105: :1257–1267. |
[5] | Englesbe MJ , Lee JS , He K , Fan L , Schaubel DE , Sheetz KH , Harbaugh CM , Holcombe SA , Campbell DA Jr , Sonnenday CJ , Wang SC . Analytic morphomics, core muscle size and surgical outcomes. Annals of Surgery (2012) ;256: (2:255–261. |
[6] | Englesbe MJ , Terjimanian MN , Lee JS , Sheetz KH , Harbaugh CM , Hussain A , Holcombe SA , Sullivan J , Campbell DA Jr , Wang SC , Sonnenday CJ . Morphometric age and surgical risk. Journal of the American College of Surgeons (2013) ;216: (5:976–985. |
[7] | Lee JS , He K , Harbaugh CM , Sonnenday CJ , Wang SC , Englesbe MJ , Eliason JL . Frailty, core muscle size, and mortality in patients undergoing open abdominal aortic aneurysm repair. Journal Vascular Surgery (2011) ;53: :912–917. |
[8] | Englesbe MJ , Patel SP , He K , Lynch RJ , Schaubel DE , Harbaugh C , Holcombe SA , Wang SC , Segev DL , Sonnenday CJ . Sarcopenia and mortality after liver transplantation. Journal American College of Surgeons (2010) ;211: :271–278. |
[9] | Miller BS , Ignatoski KM , Daignault S , Lindland C , Doherty M , Gauger PG , Hammer GD , Wang SC , Doherty GM . Worensing central sarcopenia and increasing intra-abdominal fat correlate with decreased survival in patients with adrenocortical carcinoma. World Journal of Surgery (2012) . |
[10] | Sabel MS , Terjimanian M , Conlon AS , Griffith KA , Morris AM , Mulholland MW , Englesbe MJ , Holcombe S , Wang SC . Analytic morphomic assessment of patients undergoing colectomy for colon cancer. Journal of Surgical Oncology (2013) ;108: :169–175. |
[11] | Waits SA , Kim EK , Terjimanian MN , Tishberg LM , Harbaugh CM , Sheetz KH , Sonnenday CJ , Sullivan J , Wang SC , Englesbe MJ . Morphometric age and mortality after liver transplant. JAMA Surgery (2014) ;149: (4):335–340. |
[12] | Lieffers JR , Bathe OF , Fassbender K , Winget M , Baracos VE . Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. British Journal of Cancer (2012) ;251: :981–988. |
[13] | Hollenbeck BK , Dunn RL , Wolf JS Jr , Sanda MG , Wood DP , Gilbert SM , Weizer AZ , Montie JE , Wei JT . Development and validation of the convalescence and recovery evaluation (CARE) for measuring quality of life after surgery. Quality of Life Resource (2008) ;17: :915–926. |
[14] | Sabel MS , Lee J , Cai S , Englesbe MJ , Holcombe S , Wang S . Sarcopenia as a Prognostic Factor among Patients with Stage III Melanoma. Annals of Surgical Oncology (2011) ;18: :3579–3585. |
[15] | Mualla R , Terjimanian MN , Cron DC (unpublished data) Abdominal Adiposity compared to Body Mass Index as a Predictor of Surgical Complications. Academic Surgical Congress, (2014) . |
Figures and Tables
Fig.1
Histograms of psoas muscle area and lean psoas muscle area in males & females. Total psoas muscle area in men on average was greater than women. The total psoas muscle area range in men was 1000–4200 mm2, while in women the total psoas muscle area range was 800 to 2200 mm2.
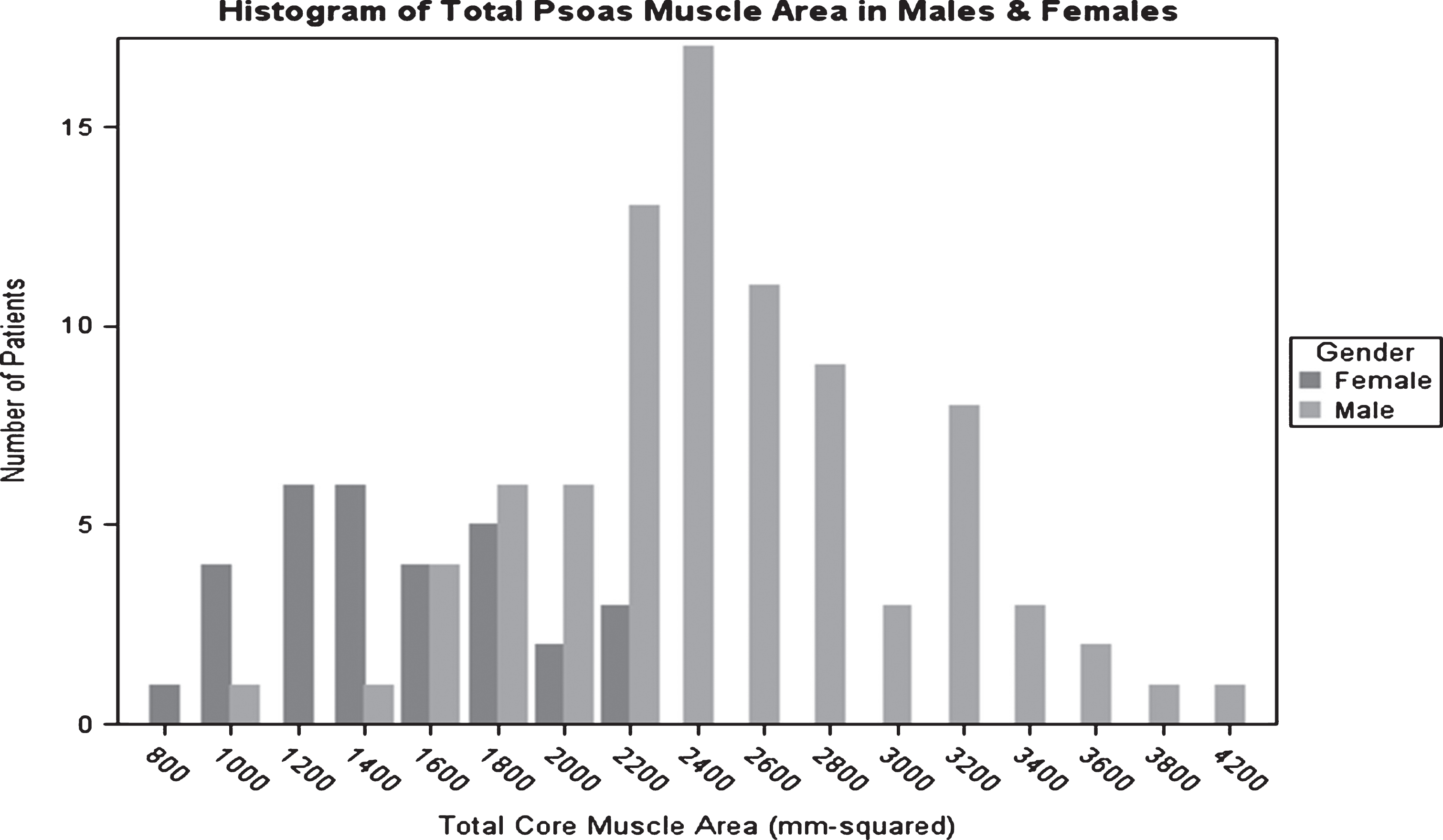
Fig.2
Variation in morphometric characteristics seen on pre-operative CT scan in two age-matched males of similar size, with similar comorbid conditions. CT on the left demonstrating high psoas muscle area, CT on the right demonstrating low psoas muscle area, both with respect to the mean.
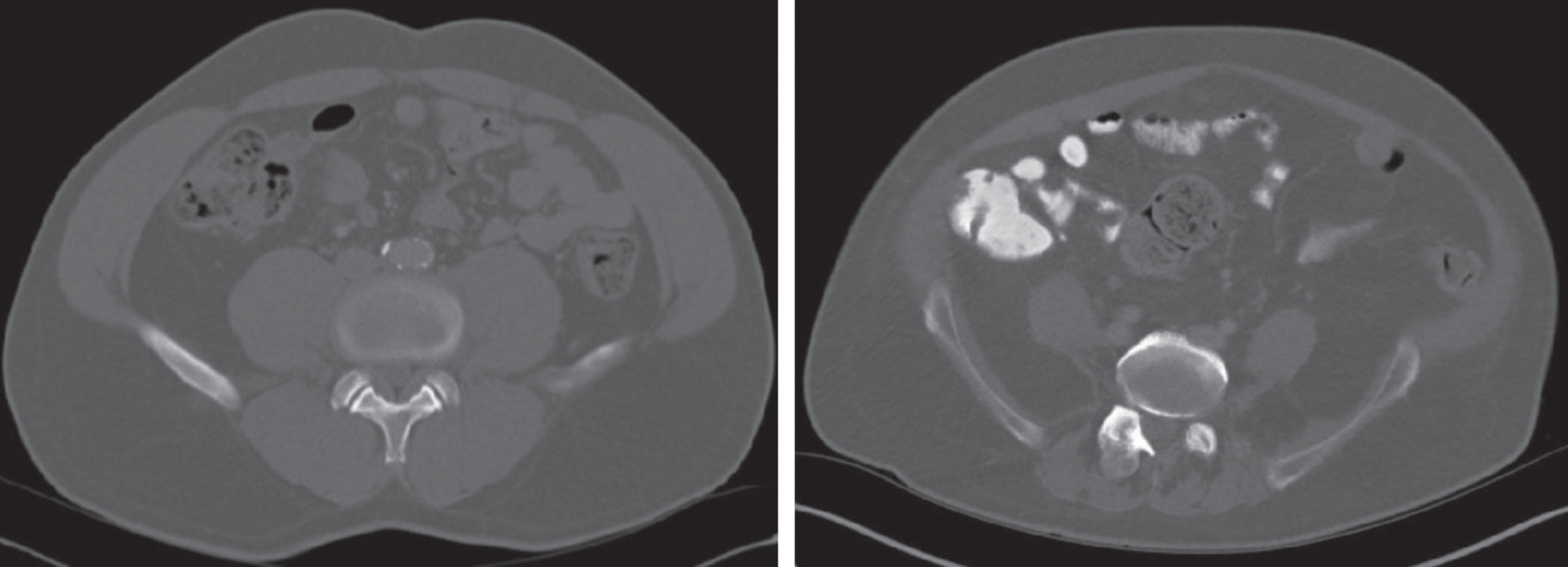
Fig.3
Changes in CARE Scores from baseline after bladder surgery among women with high and low psoas muscle area. Women with higher psoas muscle area had smaller changes in their baseline pain score and activity score compared to women with low psoas muscle area. The change in baseline pain score was statistically significant after controlling for patient age and neoadjuvant chemotherapyreceipt.
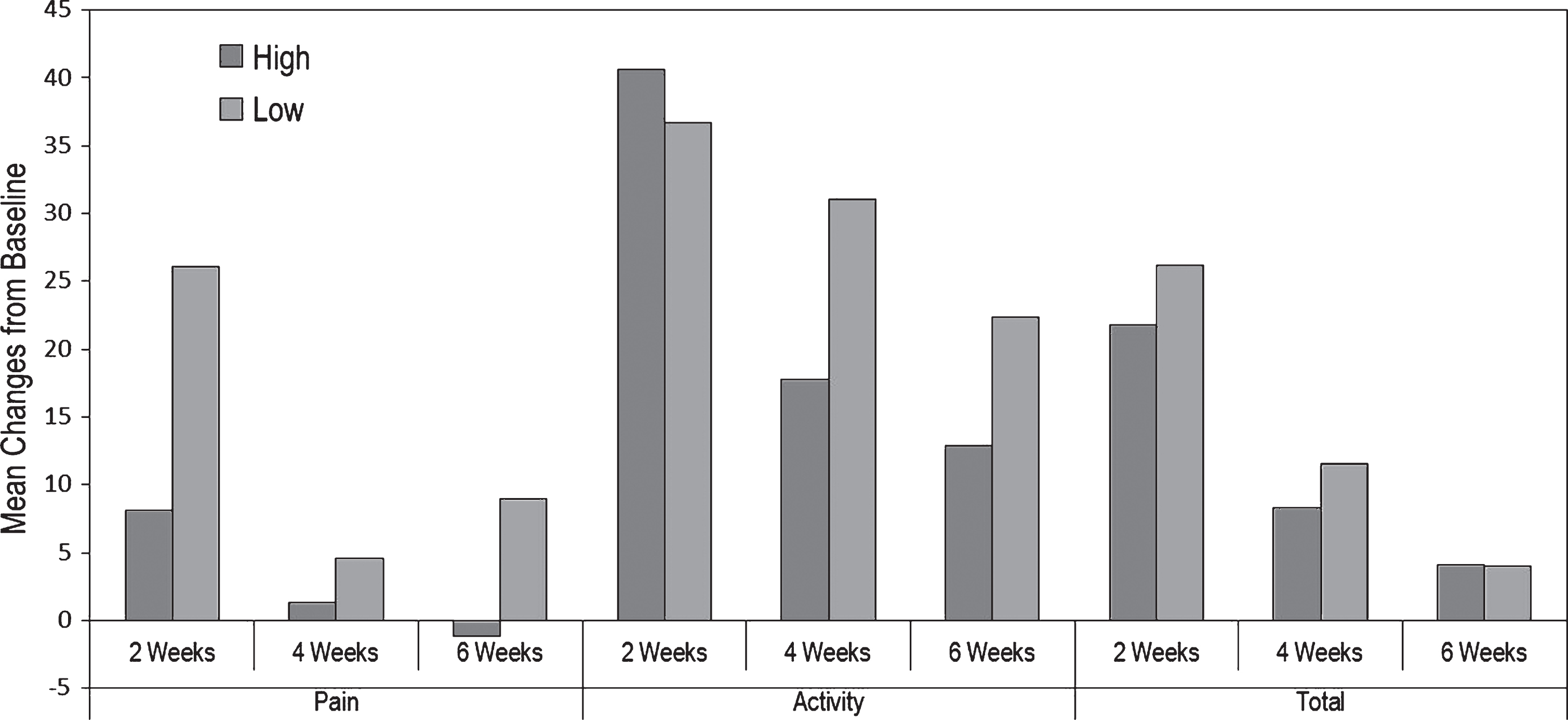
Table 1
Patient characteristics in the high versus low psoas muscle area group, stratified by gender
| Patient Characteristic | Men (n = 86) | Women (n = 31) | ||
| Low (n = 43) | High (n = 43) | Low (n = 15) | High (n = 16) | |
| Age+SD (years) | 53.6 ± 36.6 | 51.0 ± 29.3 | 56.6 ± 32.8 | 45.7 ± 44.0 |
| Race (%) | ||||
| White | 95.4 | 95.4 | 100 | 87.5 |
| Black | 2.3 | 4.7 | 0 | 12.5 |
| Hispanic | 0 | 0 | 0 | 0 |
| Asian | 0 | 0 | 0 | 0 |
| Other | 2.30 | 0 | 0 | 0 |
| ASA Score (%) | ||||
| 1 | 0 | 0 | 0 | 0 |
| 2 | 34.9 | 51.2 | 46.7 | 25 |
| 3 | 62.8 | 46.5 | 53.3 | 75 |
| 4 | 2.3 | 2.3 | 0 | 0 |
| Clinical Stage (%) | ||||
| High Grade Ta/Tis/T1 | 44.2 | 55.8 | 46.7 | 62.5 |
| T2 | 37.2 | 34.9 | 40 | 31.3 |
| T3 | 14. | 7 | 13.3 | 6.3 |
| T4 | 2.3 | 0 | 0 | 0 |
| Tx | 2.3 | 2.3 | 0 | 0 |
| Diversion Type | ||||
| Ileal Conduit | 83.7 | 55.8 | 80. | 93.8 |
| Neobladder | 16.3 | 44.2 | 20 | 6.3 |
| Neoadjuvant Chemotherapy | ||||
| Yes | 44.2 | 44.2 | 46.7 | 56.3 |
| No | 55.8 | 55.8 | 53.3 | 43.8 |




