Spotlight on: Nature, assessment, and management of laryngopharyngeal reflux
Abstract
Laryngopharyngeal reflux (LPR) is a condition that affects up to 10% of the general population. It contributes to breathing, hearing, voicing, and swallowing problems. By incorporating knowledge of this phenomenon into their practice, clinicians may better address these concerns. This Spotlight on Nature, Assessment, and Management of Laryngopharyngeal Reflux equips clinicians with a current understanding of how and why LPR occurs, and what to do about it. Practical recommendations are provided to support immediate implementation of knowledge, and to improve patient care.
1Introduction
Laryngopharyngeal reflux (LPR) is an inflammatory condition caused by the backflow of gastroduodenal reflux into the upper aerodigestive tract (Lechien, Akst, et al., 2019). When refluxate contacts aerodigestive tissues, it may cause or contribute to cough, dysphagia, dysphonia, excess throat mucous, globus sensation, heartburn, post-nasal drip, and throat clearing (Johnston et al., 2013; Krause et al., 2022; Lechien, 2023; Yeakel et al., 2023). LPR is typically encountered by ear-nose-throat (ENT) clinics, general practitioners, respiratory specialists, and speech and language therapists. This Spotlight on provides an evidence-based update on current knowledge about nature, assessment, and management of this condition. It aims to provide clinicians with contemporary knowledge, so that patients can receive the best available care.
2Nature
2.1Prevalence and risk factors
Research into LPR has expanded considerably in the last decade. Given changing definitions and understanding of this condition, its precise incidence and prevalence are unknown. An estimated 1–10% of the general population have LPR symptoms, while symptoms are present in up to 30% of patients attending ENT (Lechien, 2023). Risk factors include alcohol consumption, hiatal hernia, high body mass index (BMI), and tobacco use (Saruç et al., 2012; Spantideas et al., 2015). Identification of risk factors is problematic, because some risk factors may themselves generate LPR-like symptoms, e.g. laryngopharyngeal irritation caused by smoking (Lechien, Akst, et al., 2019).
2.2Components and mechanisms
The digestive functions of the stomach were explained by O’Connor & O’Moráin (2014). Stomach acid is at pH 1.5–3.5, where it has a role in both controlling pathogens and softening foods to make them ready for further digestion. Pepsinogen is a pro-enzyme secreted by the gastric mucosa, which converts into pepsin upon exposure to acid. Pepsin’s primary role is to break proteins into polypeptides. The stomach is protected by an alkaline-producing mucosal layer, which prevents auto-digestion of the organ.
The pharynx is pH neutral (7.0) and is easily damaged by exposure to gastric contents (Campagnolo et al., 2014). While stomach acid may directly damage the airway epithelium (Liu et al., 2020), pepsin has been demonstrated to have a significant role in reflux-related hypopharyngeal trauma. Pepsin is most strongly activated at pH 1.5–2.5, deactivates (but remains stable for up to 24 hours) at 6.5–7.0, and is not irreversibly inactivated until pH 8.0 (Johnston et al., 2007). When in the hypopharynx, pepsin binds to cells, continues to digest proteins, damages cell cohesion, and causes mitochondrial damage (Johnston et al., 2010). During repeated exposure, pepsin plays a role in the development of laryngeal malignancy (Parsel et al., 2019).
2.3Reflux subtypes
Subtypes of LPR were summarised by Liu et al. (2020), who discriminate it from gastroesophageal reflux disease (GORD/GERD). GORD tends to feature liquid acid reflux, while LPR refluxate is often gaseous, and may be acid, non-acid, or mixed, tending towards the latter two. Since LPR may be low- or non-acid, it does not always cause heartburn, and may be considered a ‘silent reflux’ (McGlashan et al., 2009; Vaezi et al., 2018). In LPR, abnormal findings are not necessarily present using oesophagogastroduodenoscopy (OGD) or standard pH-monitoring tests (Reichel & Issing, 2007; Vaezi et al., 2018) because of low-acid content. GORD events often occur at night in a recumbent position, while LPR is more usual during the day in an upright position. LPR events occur approximately 4 times per day, most commonly 2 hours after meals (Kang et al., 2023). LPR and GORD are not necessarily discrete conditions, with some authors postulating that LPR is an extra-oesophageal variant of GORD (Lien et al., 2023).
2.4Consequences and associated conditions
Laryngopharyngeal consequences of LPR include dysphagia, dysphonia, excess throat mucous, globus sensation, odynophagia, throat clearing, and throat pain (Lechien, 2023). LPR is implicated as a cause of chronic cough (Yeakel et al., 2023) and inducible laryngeal obstruction/paradoxical vocal fold movement (Franca, 2014; Shay et al., 2020).
Since LPR travels above the oesophagus and can be gaseous, it affects other upper aerodigestive structures. A systematic review identified that LPR may contribute to dental erosion and caries, though the findings were reportedly not fully reliable (Lechien, Chiesa-Estomba, et al., 2020). Burning Mouth Syndrome (BMS) is a condition characterised by ongoing or recurrent burning sensation in the mouth with no known cause. A study of individuals with BMS identified that 94% of them had LPR, and that their BMS significantly improved following LPR treatment (Lechien, Hans, et al., 2021).
Zhen et al. (2022) describe otitis media with effusion (OME) as fluid in the middle ear. Symptoms include earache, ear fullness, hearing loss, and tinnitus. These authors examined adults with OME using the Reflux Symptom Index (RSI; Belafsky et al., 2002) and tubomanometry (TMM). TMM semi-objectively measures eustachian tube patency by inducing nasopharyngeal pressure changes, then records corresponding pressure changes in the external ear. The authors identified that higher RSI scores were significantly associated with worse TMM scores. They hypothesised that LPR causes fluid and microenvironment changes, adversely affecting eustachian tube function.
Whether LPR is associated with rhinosinusitis is unclear. Many studies examining the relationship between these conditions fail to adequately discriminate between LPR and GORD (Lechien et al., 2023). One study demonstrated a positive relationship between allergic rhinitis and LPR presence (Alharethy et al., 2018), while another identified that GORD is significantly associated with the presence of post-nasal drip (Morimoto et al., 2021).
Liu et al. (2023) noted that the effects of LPR on quality of life are complicated by poor discrimination between LPR and GORD. They reported that while GORD adversely affects quality of life, researchers have not yet adequately measured the impact of LPR on individuals’ lives.
3Assessment
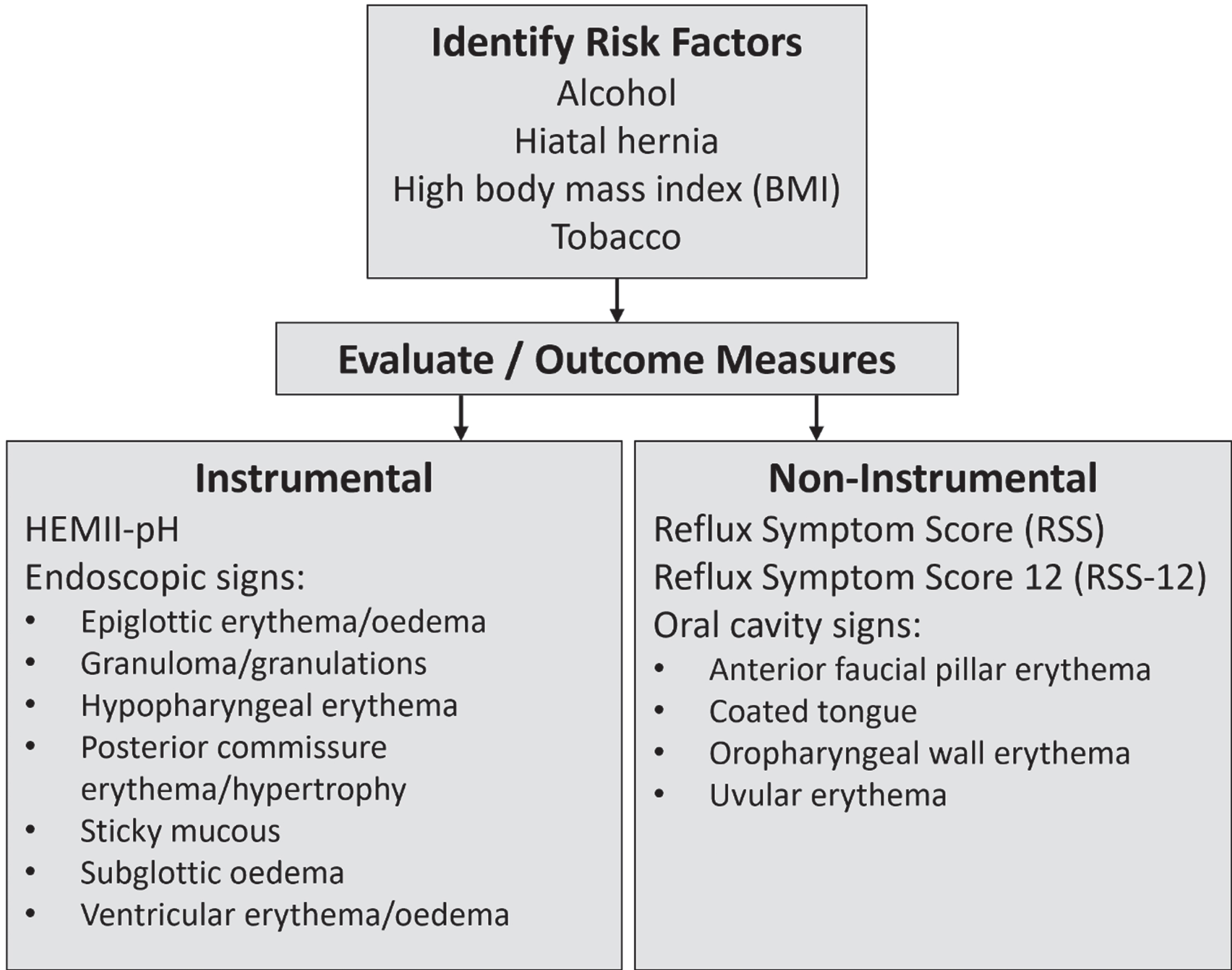
Various means for evaluating the presence of LPR have been proposed based on different characteristics and manifestations of the condition. While instrumental measurement may be required to examine internal structures, oral cavity inspection can also contribute to LPR diagnosis. Those with this condition may have coated tongue, as well as erythema of the anterior faucial pillars, oropharyngeal wall, and uvula (Lechien, Bobin, Muls, et al., 2021).
3.1Instrumental
Historically, 24-hour pH monitoring was used to diagnose LPR. This is suboptimal, since LPR may be low- or non-acid, leading to false positive rates of 20–50% (Fuchs et al., 2018; Lechien, Mouawad, et al., 2021). Additionally, pH monitoring measures the oesophagus, while LPR affects the laryngopharynx. Hypopharyngeal-esophageal multichannel intraluminal impedance with dual pH (HEMII-pH) has therefore replaced traditional pH monitoring as a modern standard for LPR diagnosis (Borges et al., 2019).
This technique utilises impedance sensors within the hypopharynx and the oesophagus. Sensors generate an electric current between pairs of electrodes. Swallowed or refluxed materials change electrode conductivity, with higher acid concentrations leading to greater conductivity. The device is therefore capable of detecting non-, low-, or high-acid reflux events. Two pH monitors positioned at the upper and lower oesophagus provide absolute pH values. A limitation of HEMII-pH (and other pH-monitoring techniques) is that they do not detect pepsin presence or concentration.
Restech (Respiratory Technology Corporation, Houston, USA) is a pH-monitoring probe that is passed transnasally and fixed in place once it reaches 1 cm below the uvula. The probe connects to an ambulatory monitoring device. A study comparing this technique to HEMII-pH in patients with LPR found that they agreed significantly on the total number of postprandial reflux events and events with pH <5 (Vance et al., 2021). Restech detected more events at pH 5–7, while HEMII-pH detected more events at pH <4. Restech also detected a higher number of reflux events than HEMII-pH. The authors noted that differences between devices could be due to the instruments measing pH at different anatomical locations, as well as the fact that Restech may detect pH changes that are not due to reflux (e.g. inhaled acids). In sites that utilise traditional pH-monitoring, Restech has been recommended as an adjunctive diagnostic tool to inform clinical decision-making (Fuchs et al., 2018).
Endoscopically, the appearance of the laryngopharynx may be affected by LPR, depending on the reflux subtype and frequency of episodes. Two studies identified abnormal laryngopharyngeal features in individuals diagnosed with LPR by HEMII-pH (Lechien, Bobin, Muls, et al., 2021; Lee et al., 2018). Features included: epiglottic erythema (and/or oedema), granuloma/granulations, hypopharyngeal wall erythema, laryngopharyngeal sticky mucous, posterior commissure erythema and hypertrophy, subglottic oedema, ventricular erythema (and/or oedema).
Peptest (RD Biomed Limited, Hull, UK) was developed as a means of testing for pepsin presence within saliva to diagnose LPR. It has the advantage of being non-invasive and portable. A systematic review (Guo et al., 2021) of studies investigating its diagnostic properties found a pooled sensitivity of 65% (95% CI 49% –73%) and specificity of 74% (95% CI 50% –90%). The review included any studies of people with LPR or GORD, limiting its applicability to LPR alone. The authors also noted that not all included studies used HEMII-pH as a reference standard.
Digital reflux scintigraphy permits direct visualisation of reflux (Falk et al., 2015). (Park et al., 2021) studied this technique in LPR patients, who fasted for 12 hours, then ingested radio-labelled technetium-99 m (Tc-99 m) phytate. Participants were imaged in standing and supine position over several hours. Imaging identified the presence of Tc-99 m phytate in the sinuses, laryngopharynx, and lungs. While the scintigraphy’s strength lies in its ability to detect regions affected by reflux, it does not detect pepsin or acid concentrations, and is a lengthy procedure.
3.2Patient-reported outcome measures (PROMs)
Given the burden and potential invasiveness of instrumental LPR evaluation, several PROMs were developed to identify LPR presence, measure impact on daily living, and capture response to treatment. One of the most commonly reported tools is the Reflux Symptom Index (Belafsky et al., 2002). This 9-item questionnaire asks participants to rate their experience of LPR-induced symptoms. According to the authors, RSI scores >13 indicate potential LPR. While this tool is widely used in both clinical and research settings, it is significantly limited by its validation using a small sample size, use of oesophageal pH-monitoring as a reference standard and overlap with symptoms caused by other conditions.
Given advances in LPR knowledge, the Reflux Symptom Score (RSS; Lechien, Bobin, et al., 2020) was developed using a robust sample size and HEMII-pH as a reference standard. This questionnaire rates frequency and severity of 22 different LPR-associated symptoms, with scores >13 suggesting LPR (sensitivity 94.5%, specificity 81%). The tool also allows participants to report symptoms not captured by the tool and includes a quality-of-life outcome measure. The tool’s authors reported strong reliability, validity, and responsiveness to change over time. The Reflux Symptom Score-12 (Lechien, Bobin, Rodriguez, et al., 2021) was reduced to twelve items, while maintaining strong diagnostic accuracy (sensitivity 94.5%, specificity 86.2%). RSS and RSS-12 were originally developed in French, and while they have been translated into English, no validation has yet occurred in this language.
4Management
4.1Pharmaceutical
Proton pump inhibitor (PPI) medications are commonly used for reflux because they supress gastric acid secretion (Tanus-Santos & Pinheiro, 2019). In patients with symptoms of LPR, they offer no benefit (O’Hara et al., 2021), or only mild benefit (Lechien, Saussez, et al., 2019). PPIs can cause side-effects including increased risk of dementia, kidney diseases, micronutrient malabsorption, and susceptibility to bacterial infection (Tanus-Santos & Pinheiro, 2019).
Liquid alginate suspensions have proven effective for LPR management (Pizzorni et al., 2022). A landmark study using Gaviscon Advance (Reckitt Benckiser, Slough, UK) examined the benefits of this medication over a six-month period (McGlashan et al., 2009). Gaviscon Advance inhibits pepsin activity and interacts with gastric contents to form a barrier that prevents reflux episodes. It is available over the counter in many jurisdictions. Participants took 10 mls of Gaviscon Advance four times per day; once after each main meal and once again before bed. There were significant improvements in reflux symptom scores and clinical findings after one, three, and six months. A limitation of existing research using alginates is that the minimum period for administration of this medication to identify change has not been firmly established. (McGlashan et al., 2009) identified improvements after one month, but clinicians should monitor patients on a weekly basis, since relief from LPR may happen sooner.
4.2Diet and lifestyle
Certain foods and drinks have been identified as refluxogenic. Lechien, Saussez, et al. (2020) identified a list of foods and beverages for those with LPR to favour and avoid. Refluxogenic ratings were based on a literature review and expert consensus, which identified that high alcohol percentage, high caffeine levels, carbonation, high fat, low pH levels, and high spice concentration all contribute to reflux (Lechien et al., 2019). While mental health difficulties and stress are known to exacerbate GORD (He et al., 2022), no studies have yet identified the extent to which these contribute to LPR. A recent study identified that anxiety is a risk factor for LPR, but this research utilised RSI to diagnose LPR, potentially affecting its validity (Gui et al., 2023).
4.3Surgical
When pharmaceutical, dietary and lifestyle management fail, specialists may recommend surgical intervention. Nissen fundoplication involves wrapping the upper stomach around the lower oesophagus to limit gastric reflux and was found to be effective at reducing both LPR and GORD (Morice et al., 2022; Trad et al., 2012). Magnetic sphincter augmentation (MSA) has been proposed as an alternative to fundoplication. Magnetic beads are installed into the lower oesophagus and improve lower oesophageal sphincter resting pressure and closure length (Dunn et al., 2020). MSA shows comparable improvements to fundoplication, with improved ability to maintain belching and vomiting versus fundoplication (Schoppmann, 2023).
5Care recommendations
The following recommendations are based on literature review, author’s experience, and reflect published guidelines (Kamal et al., 2023; Lechien, Saussez, et al., 2020).
5.1Evaluation
Figure 1 summarises the evaluation process. Clinicians should keep an open mind about the potential presence of LPR during case history, paying particular attention to risk factors. While doing so, they should also consider co-existing or alternative explanations for reflux-like signs and symptoms. For example, rhinosinusitis could be caused by allergy, chronic cough by asthma. If LPR is suspected, RSS (Lechien, Bobin, et al., 2020) or RSS-12 (Lechien, Bobin, Rodriguez, et al., 2021) can be administered. Most clinics will not have HEMII-pH, but oral cavity examination can be conducted, and laryngeal endoscopy may be available. Evaluation tools may also serve as outcome measures to determine intervention effectiveness.
Fig. 1
Evaluation of LPR.
5.2Management
Figure 2 presents an overview of suggested management. If LPR is identified, but co-existing conditions might exist, additional investigation and management by other specialists may supplement care. This does not necessarily mean that LPR should remain untreated, so clinical judgement should be exercised. A period of ‘diagnostic therapy’ is useful to ensure that symptoms are reflux related. Gaviscon Advance for up to one month ought to provide relief from LPR symptoms, but clinicians should observe warnings labels and exercise caution if patients have existing heart, kidney, or liver disease. PPI medication may also be prescribed but should be carefully considered given its negligible benefits to those who have non- or low-acid LPR.
Fig. 2
Management of LPR.
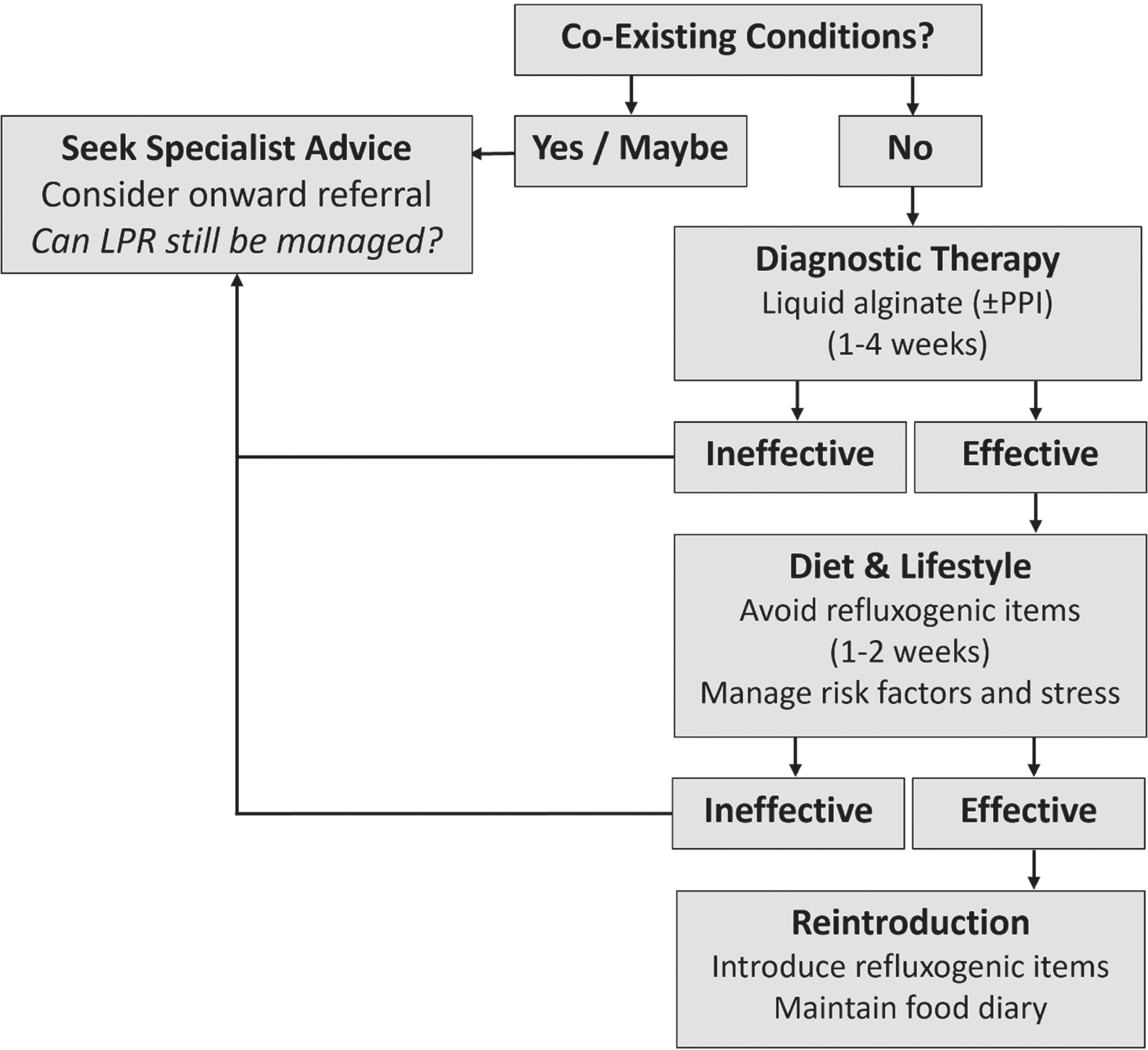
If no relief is obtained, specialist referral may identify conditions like gastric infection, hiatal hernia, or oesophageal dysmotility for medical or surgical follow-up. If Gaviscon Advance is successful, this can be stopped. Patients then consume a low refluxogenic diet for at least one week. A list of refluxogenic foods and beverages is provided by Lechien, Saussez, et al. (2020). Clinicians should support clients to simultaneously manage risk factors (e.g. smoking cessation, weight loss) and stress. If reflux symptoms return, this may indicate a medical cause and specialist investigations may once again be helpful.
Higher refluxogenic items can be reintroduced one-by-one. Individuals should consume large amounts of the food or beverage for two or three days to identify whether it is problematic for them, and document this in a food diary. If the item is problematic, it should be eliminated again until the trial period is over. Ultimately, the food diary will allow individuals with LPR to make informed choices about what they can and cannot consume. For those who obtain only partial relief through diet and lifestyle management, a reduced dose of alginate could be considered in the long-term. Finally, if LPR symptoms are adequately managed, medical practitioners could consider de-prescribing PPIs.
6Knowledge limitations and future directions
While LPR management has improved, knowledge gaps limit contemporary management. Crucially, many studies fail to discriminate LPR from GORD, and fail to use modern standards for LPR diagnosis, which can lead to conflicting evidence. While HEMII-pH is now used as a reference standard, it is not an agreed gold standard, and fails to provide information captured by other techniques like pepsin measurement and scintigraphy.
The impact of LPR on pulmonary function has been under-reported, and its role in chronic cough has largely been addressed from a laryngeal perspective. While some literature has examined how LPR contributes to oesophageal dysphagia, the oropharynx is also affected by reflux, yet dysphagia in this region has not been adequately characterised. Lack of information about impact on quality-of-life suggests that current literature has a medical focus but fails to capture lived experiences.
In terms of pharmaceutical management, it would be helpful to know ideal alginate dosage and length of treatment required to obtain positive outcomes. Pharmaceutical, dietary, and lifestyle management recommendations have not yet been conclusively tested, so it remains difficult to know when surgical management (as a last resort) should be advised.
7Conclusions
LPR is a condition that is commonly encountered by those working in communication and swallowing. This article provides a current and evidence-based overview of mechanisms of action, assessment and management. Clinicians should consider incorporating these into their practice to optimise patient care. Future research should focus on creation of a gold standard for LPR diagnosis, and should identify best management techniques and pathways of care.
Acknowledgments
The author has no acknowledgments.
Conflict of interest
Given his role as Editorial Board member, Ciarán Kenny had no involvement in nor access to information regarding the peer review of this article.
References
1 | Alharethy, S. , Baqays, A. , Mesallam, T. A. , Syouri, F. , Al Wedami, M. , Aldrees, T. , AlQabbani, A. ((2018) ). Correlation between allergic rhinitis and laryngopharyngeal reflux. BioMed Research International, 2018: , 1–6. https://doi.org/10.1155/2018/2951928 |
2 | Belafsky, P. C. , Postma, G. N. , Koufman, J. A. ((2002) ). Validity and reliability of the reflux symptom index (RSI). Journal of Voice, 16: (2), 274–277. https://ac.els-cdn.com/S0892199702000978/1-s2.0-S0892199702000978-main.pdf?tid=9574bb45-aa2f-4b67-b53e-e753c03d21f3&acdnat=1551370283b7e4dc315364c9e18d44e101ff5b21d5 |
3 | Borges, L. F. , Chan, W. W. , Carroll, T. L. ((2019) ). Dual pH probes without proximal esophageal and pharyngeal impedance may be deficient in diagnosing LPR. Journal of Voice, 33: (5), 697–703. https://doi.org/10.1016/j.jvoice.2018.03.008 |
4 | Campagnolo, A. M. , Priston, J. , Thoen, R. H. , Medeiros, T. , Assuncao, A. R. ((2014) ). Laryngopharyngeal reflux: Diagnosis, treatment, and latest research. International Archives of Otorhinolaryngology, 18: (2), 184–191. https://doi.org/10.1055/s-0033-1352504 |
5 | Dunn, C. , Bildzukewicz, N. , Lipham, J. ((2020) ). Magnetic sphincter augmentation for gastroesophageal reflux disease. Gastrointestinal Endoscopy Clinics of North America, 30: (2), 325–342. https://doi.org/10.1016/j.giec.2019.12.010 |
6 | Falk, G. L. , Beattie, J. , Ing, A. , Falk, S. E. , Magee, M. , Burton, L. , Van der Wall, H. ((2015) ). Scintigraphy in laryngopharyngeal and gastroesophageal reflux disease: A definitive diagnostic test? World Journal of Gastroenterology, 21: (12), 3619–3627. https://doi.org/10.3748/wjg.v21.i12.3619 |
7 | Franca, M. C. ((2014) ). Differential diagnosis in paradoxical vocal fold movement (PVFM): An interdisciplinary task. International Journal Of Pediatric Otorhinolaryngology, 78: (12), 2169–2173. https://doi.org/10.1016/j.ijporl.2014.10.003 |
8 | Fuchs, H. F. , Muller, D. T. , Berlth, F. , Maus, M. K. , Fuchs, C. , Dubbers, M. , Schroder, W. , Bruns, C. J. , Leers, J. M. ((2018) ). Simultaneous laryngopharyngeal pH monitoring (Restech) and conventional esophageal pH monitoring-correlation using a large patient cohort of more than 100 patients with suspected gastroesophageal reflux disease. Diseases of the Esophagus, 31: (10), 1–8. https://doi.org/10.1093/dote/doy018 |
9 | Gui, C. , Xiaoxuan, K. , Xiaofen, W. , Jinfeng, Y. , Mei, R. , Yaqian, T. , Saixuan, Y. , Wenjing, L. , Lijuan, S. , Xiaowen, Z. ((2023) ). Psychological factors, lifestyles, and habits of patients with laryngopharyngeal reflux:Amulticenter survey. B-ENT, 19: (3), 170–174. https://doi.org/10.5152/B-ENT.2023.231290 |
10 | Guo, Z. , Jiang, J. , Wu, H. , Zhu, J. , Zhang, S. , Zhang, C. ((2021) ). Salivary peptest for laryngopharyngeal reflux and gastroesophageal reflux disease: A systemic review and meta-analysis. Medicine (Baltimore), 100: (32), e26756. https://doi.org/10.1097/MD.0000000000026756 |
11 | He, M. , Wang, Q. , Yao, D. , Li, J. , Bai, G. ((2022) ). Association between psychosocial disorders and gastroesophageal reflux disease: A systematic review and meta-analysis. Journal of Neurogastroenterology and Motility, 28: (2), 212–221. https://doi.org/10.5056/jnm21044 |
12 | Johnston, N. , Dettmar, P. W. , Bishwokarma, B. , Lively, M. O. , Koufman, J. A. ((2007) ). Activity/stability of human pepsin: Implications for reflux attributed laryngeal disease. The Laryngoscope, 117: (6), 1036–1039. https://doi.org/10.1097/MLG.0b013e31804154c3 |
13 | Johnston, N. , Dettmar, P. W. , Strugala, V. , Allen, J. E. , Chan, W. W. ((2013) ). Laryngopharyngeal reflux and GERD. Annals Of The New York Academy Of Sciences, 1300: , 71–79. https://doi.org/10.1111/nyas.12237 |
14 | Johnston, N. , Wells, C. W. , Samuels, T. L. , Blumin, J. H. ((2010) ). Rationale for targeting pepsin in the treatment of reflux disease. Annals of Otology, Rhinology & Laryngology, 119: (8), 547–558. https://doi.org/10.1177/000348941011900808 |
15 | Kamal, A. N. , Dhar, S. I. , Bock, J. M. , Clarke, J. O. , Lechien, J. R. , Allen, J. , Belafsky, P. C. , Blumin, J. H. , Chan, W. W. , Fass, R. , Fisichella, P. M. , Marohn, M. , O’Rourke, A. K. , Postma, G. , Savarino, E. V. , Vaezi, M. F. , Carroll, T. L. , Akst, L. M. ((2023) ). Best practices in treatment of laryngopharyngeal reflux disease: A multidisciplinary modified delphi study. Digestive Diseases and Sciences, 68: (4), 1125–1138. https://doi.org/10.1007/s10620-022-07672-9 |
16 | Kang, J. W. , Lee, Y. C. , Ko, S. G. , Eun, Y. G. ((2023) ). The key timing of pharyngeal reflux in patients with laryngopharyngeal reflux. Auris Nasus Larynx, 50: (4), 565–570. https://doi.org/10.1016/j.anl.2022.11.002 |
17 | Krause, A. J. , Walsh, E. H. , Weissbrod, P. A. , Taft, T. H. , Yadlapati, R. ((2022) ). An update on current treatment strategies for laryngopharyngeal reflux symptoms. Annals of the New York Academy of Sciences, 1510: (1), 5–17. https://doi.org/10.1111/nyas.14728. |
18 | Lechien, J. R. ((2023) ). Sensitivity, specificity, and predictive values of laryngopharyngeal reflux symptoms and signs in clinical practice. Otolaryngology-Head & Neck Surgery, 169: (1), 97–104. https://doi.org/10.1177/01945998221121822 |
19 | Lechien, J. R. , Akst, L. M. , Hamdan, A. L. , Schindler, A. , Karkos, P. D. , Barillari, M. R. , Calvo-Henriquez, C. , Crevier-Buchman, L. , Finck, C. , Eun, Y. -G. , Saussez, S. , Vaezi, M. F. ((2019) ). Evaluation and management of laryngopharyngeal reflux disease: State of the art review. Otolaryngology-Head & Neck Surgery, 160: (5), 762–782. https://doi.org/10.1177/0194599819827488 |
20 | Lechien, J. R. , Bobin, F. , Mouawad, F. , Zelenik, K. , Calvo-Henriquez, C. , Chiesa-Estomba, C. M. , Enver, N. , Nacci, A. , Barillari, M. R. , Schindler, A. , Crevier-Buchman, L. , Hans, S. , Simeone, V. , Wlodarczyk, E. , Harmegnies, B. , Remacle, M. , Rodriguez, A. , Dequanter, D. , Eisendrath, P. , Saussez, S. ((2019) ). Development of scores assessing the refluxogenic potential of diet of patients with laryngopharyngeal reflux. European Archives of Oto-Rhino-Laryngology, 276: (12), 3389–3404. https://doi.org/10.1007/s00405-019-05631-1 |
21 | Lechien, J. R. , Bobin, F. , Muls, V. , Mouawad, F. , Dapri, G. , Dequanter, D. , Horoi, M. , Thill, M. P. , Rodriguez Ruiz, A. , Saussez, S. ((2021) ). Changes of laryngeal and extralaryngeal symptoms and findings in laryngopharyngeal reflux patients. Laryngoscope, 131: (6), 1332–1342. https://doi.org/10.1002/lary.28962 |
22 | Lechien, J. R. , Bobin, F. , Muls, V. , Thill, M. P. , Horoi, M. , Ostermann, K. , Huet, K. , Harmegnies, B. , Dequanter, D. , Dapri, G. , Maréchal, M. T. , Finck, C. , Rodriguez Ruiz, A. , Saussez, S. ((2020) ). Validity and reliability of the reflux symptom score. Laryngoscope, 130: (3), E98–e107. https://doi.org/10.1002/lary.28017 |
23 | Lechien, J. R. , Bobin, F. , Rodriguez, A. , Dequanter, D. , Muls, V. , Huet, K. , Harmegnies, B. , Crevier-Buchman, L. , Hans, S. , Saussez, S. , Carroll, T. L. ((2021) ). Development and validation of the short version of the reflux symptom score: Reflux symptom score-12. Otolaryngology-Head & Neck Surgery, 164: (1), 166–174. https://doi.org/10.1177/0194599820941003 |
24 | Lechien, J. R. , Chiesa-Estomba, C. M. , Calvo Henriquez, C. , Mouawad, F. , Ristagno, C. , Barillari, M. R. , Schindler, A. , Nacci, A. , Bouland, C. , Laino, L. , Saussez, S. ((2020) ). Laryngopharyngeal reflux, gastroesophageal reflux and dental disorders: A systematic review. PLoS One, 15: (8), e0237581. https://doi.org/10.1371/journal.pone.0237581 |
25 | Lechien, J. R. , Hans, S. , De Marrez, L. G. , Dequanter, D. , Rodriguez, A. , Muls, V. , Ben Abdelouahed, F. , Evrard, L. , Maniaci, A. , Saussez, S. , Bobin, F. ((2021) ). Prevalence and features of laryngopharyngeal reflux in patients with primary burning mouth syndrome. Laryngoscope, 131: (10), E2627–E2633. https://doi.org/10.1002/lary.29604 |
26 | Lechien, J. R. , Mouawad, F. , Bobin, F. , Bartaire, E. , Crevier-Buchman, L. , Saussez, S. ((2021) ). Review of management of laryngopharyngeal reflux disease. European Annals Of Otorhinolaryngology, Head And Neck Diseases, 138: (4), 257–267. https://doi.org/10.1016/j.anorl.2020.11.002 |
27 | Lechien, J. R. , Saussez, S. , Hopkins, C. ((2023) ). Association between laryngopharyngeal reflux, gastroesophageal reflux and recalcitrant chronic rhinosinusitis: A systematic review. Clinical Otolaryngology, 48: (4), 501–514. https://doi.org/10.1111/coa.14047 |
28 | Lechien, J. R. , Saussez, S. , Muls, V. , Barillari, M. R. , Chiesa-Estomba, C. M. , Hans, S. , Karkos, P. D. ((2020) ). Laryngopharyngeal reflux: A state-of-the-art algorithm management for primary care physicians. Journal of Clinical Medicine, 9: (11). https://doi.org/10.3390/jcm9113618 |
29 | Lechien, J. R. , Saussez, S. , Schindler, A. , Karkos, P. D. , Hamdan, A. L. , Harmegnies, B. , De Marrez, L. G. , Finck, C. , Journe, F. , Paesmans, M. , Vaezi, M. F. ((2019) ). Clinical outcomes of laryngopharyngeal reflux treatment: A systematic review and meta-analysis. The Laryngoscope, 129: (5), 1174–1187. https://doi.org/10.1002/lary.27591 |
30 | Lee, Y. C. , Kwon, O. E. , Park, J. M. , Eun, Y. G. ((2018) ). Do laryngoscopic findings reflect the characteristics of reflux in patients with laryngopharyngeal reflux? Clinical Otolaryngology, 43: (1), 137–143. https://doi.org/10.1111/coa.12914 |
31 | Lien, H. C. , Lee, P. H. , Wang, C. C. ((2023) ). Diagnosis of laryngopharyngeal reflux: Past, present, and future-A minireview. Diagnostics (Basel), 13: (9). https://doi.org/10.3390/diagnostics13091643 |
32 | Liu, D. , Qian, T. , Sun, S. , Jiang, J. J. ((2020) ). Laryngopharyngeal reflux and inflammatory responses in mucosal barrier dysfunction of the upper aerodigestive tract. Journal of Inflammation Research, 13: , 1291–1304. https://doi.org/10.2147/JIR.S282809 |
33 | Liu, K. , Krause, A. , Yadlapati, R. ((2023) ). Quality of life and laryngopharyngeal reflux. Digestive Diseases and Sciences, 79: (1), 52–57. https://doi.org/10.1007/s10620-023-08027-8 |
34 | McGlashan, J. A. , Johnstone, L. M. , Sykes, J. , Strugala, V. , Dettmar, P. W. ((2009) ). The value of a liquid alginate suspension (Gaviscon Advance) in the management of laryngopharyngeal reflux. European Archives of Oto-rhino-laryngology, 266: (2), 243–251. https://doi.org/10.1007/s00405-008-0708-7 |
35 | Morice, D. , Elhassan, H. A. , Myint-Wilks, L. , Barnett, R. E. , Rasheed, A. , Collins, H. , Owen, A. , Hughes, K. , McLeod, R. ((2022) ). Laryngopharyngeal reflux: Is laparoscopic fundoplication an effective treatment? The Annals of The Royal College of Surgeons of England, 104: (2), 79–87. https://doi.org/10.1308/rcsann.2021.0046 |
36 | Morimoto, C. , Matsumoto, H. , Nagasaki, T. , Kanemitsu, Y. , Ishiyama, Y. , Sunadome, H. , Oguma, T. , Ito, I. , Murase, K. , Kawaguchi, T. , Tabara, Y. , Niimi, A. , Muro, S. , Matsuda, F. , Chin, K. , Hirai, T. ((2021) ). Gastroesophageal reflux disease is a risk factor for sputum production in the general population: The Nagahama study. Respiratory Research, 22: (1). https://doi.org/10.1186/s12931-020-01601-y |
37 | O’Connor, A. , O’Moráin, C. ((2014) ). Digestive function of the stomach. Digestive Diseases, 32: (3), 186–191. https://doi.org/10.1159/000357848 |
38 | O’Hara, J. , Stocken, D. D. , Watson, G. C. , Fouweather, T. , McGlashan, J. , MacKenzie, K. , Carding, P. , Karagama, Y. , Wood, R. , Wilson, J. A. ((2021) ) Use of proton pump inhibitors to treat persistent throat symptoms: Multicentre, double blind, randomised, placebo controlled trial, BMJ 372: m4903. https://doi.org/10.1136/bmj.m4903 |
39 | Park, J. S. , Khoma, O. , Burton, L. , Van der Wall, H. , Falk, G. L. ((2021) ). A new diagnostic paradigm for laryngopharyngeal reflux disease: Correlation of impedance-pH monitoring and digital reflux scintigraphy results. European Archives of Oto-rhino-laryngology, 278: (6), 1917–1926. https://doi.org/10.1007/s00405-021-06658-z |
40 | Parsel, S. M. , Wu, E. L. , Riley, C. A. , McCoul, E. D. ((2019) ). Gastroesophageal and laryngopharyngeal reflux associated with laryngeal malignancy: A systematic review and metaanalysis. Clinical Gastroenterology and Hepatology, 17: (7), 1253–1264.e1255. https://doi.org/10.1016/j.cgh.2018.10.028 |
41 | Pizzorni, N. , Ambrogi, F. , Eplite, A. , Rama, S. , Robotti, C. , Lechien, J. , Schindler, A. ((2022) ). Magnesium alginate versus proton pump inhibitors for the treatment of laryngopharyngeal reflux: A non-inferiority randomized controlled trial. European Archives of Oto-Rhino-Laryngology, 279: (5), 2533–2542. https://doi.org/10.1007/s00405-021-07219-0 |
42 | Reichel, O. , Issing, W. J. ((2007) ). Should patients with pH-documented laryngopharyngeal reflux routinely undergo oesophagogastroduodenoscopy? A retrospective analysis. The Journal of Laryngology & Otology, 121: (12), 1165–1169. https://doi.org/10.1017/S0022215107000680 |
43 | Saruc M. , Aksoy, E. A. , Vardereli, E. , Karaaslan, M. , Cicek, B. , Ince, U. , Oz, F. , Tözün, N. ((2012) ). Risk factors for laryngopharyngeal reflux. European Archives of Oto-Rhino-Laryngology, 269: (4), 1189–1194. https://doi.org/10.1007/s00405-011-1905-3 |
44 | Schoppmann, S. F. ((2023) ). Is magnetic sphincter augmentation indicated in patients with laryngopharyngeal reflux? Diseases of the Esophagus, 36: (Supplement 1). https://doi.org/10.1093/dote/doad012 |
45 | Shay, E. O. , Sayad, E. , Milstein, C. F. ((2020) ). Exercise-induced laryngeal obstruction (EILO) in children and young adults: From referral to diagnosis. Laryngoscope, 130: (6), E400–E406. https://doi.org/10.1002/lary.28276 |
46 | Spantideas, N. , Drosou, E. , Bougea, A. , Assimakopoulos, D. ((2015) ). Laryngopharyngeal reflux disease in the Greek general population, prevalence and risk factors. BMC Ear, Nose and Throat Disorders, 15: (7). https://doi.org/10.1186/s12901-015-0020-2 |
47 | Tanus-Santos, J. E. , Pinheiro, L. C. ((2019) ). Proton pump inhibitors: New mechanisms of action. Basic & Clinical Pharmacology & Toxicology, 125: (2), 87–88. https://doi.org/10.1111/bcpt.13237 |
48 | Trad, K. S. , Turgeon, D. G. , Deljkich, E. ((2012) ). Long-term outcomes after transoral incisionless fundoplication in patients with GERD and LPR symptoms. Surgical Endoscopy, 26: (3), 650–660. https://doi.org/10.1007/s00464-011-1932-6 |
49 | Vaezi, M. F. , Katzka, D. , Zerbib, F. ((2018) ). Extraesophageal Symptoms and Diseases Attributed to GERD: Where is the Pendulum Swinging Now. Clinical Gastroenterology and Hepatology, 16: (7), 1018–1029. https://doi.org/10.1016/j.cgh.2018.02.001 |
50 | Vance, D. , Park, J. , Alnouri, G. , Turner, R. R. , Daggumati, S. , Ferster, A. P. O. , Ahmad, A. , Lyons, K. , Ross, J. , Russell, K. , Wu, W. , Sataloff, R. T. ((2023) ). Diagnosing laryngopharyngeal reflux: A comparison between 24-hour pH-impedance testing and pharyngeal probe (Restech) testing, with introduction of the sataloff score. Journal of Voice, 37: (5), 737–747. https://doi.org/10.1016/j.jvoice.2021.04.002 |
51 | Yeakel, H. , Balouch, B. , Vontela, S. , Alnouri, G. , Sataloff, R. T. ((2023) ). The relationship between chronic cough and laryngopharyngeal reflux. Journal of Voice, 37: (2), 245–250. https://doi.org/10.1016/j.jvoice.2020.11.011 |
52 | Zhen, Z. , Zhao, T. , Wang, Q. , Zhang, J. , Zhong, Z. ((2022) ). Laryngopharyngeal reflux as a potential cause of Eustachian tube dysfunction in patients with otitis media with effusion. Frontiers in Neurology, 13: , 1024743. https://doi.org/10.3389/fneur.2022.1024743 |




