Utility of side-lying posture in a patient with severe dysphagia secondary to oropharyngeal cancer surgery: A single case report
Abstract
INTRODUCTION:
Few studies have documented the utility of side-lying in dysphagia management. We report on a patient who benefitted from the side-lying posture for safe and efficient oral intake.
PATIENT:
The patient underwent resections of the left tongue base, the left lateral pharyngeal wall, and a left marginal mandibulectomy for oropharyngeal cancer. The Videofluoroscopic Swallowing Study (VFSS) on Postoperative Day (POD) 10 confirmed significant pyriform sinus residue and post-swallow aspiration. Techniques including bolus modification, the 45-degree reclining position, head rotation to the left, and the Mendelsohn maneuver did not prevent post-swallow aspiration of severe pyriform sinus residue. Instead of the 45-degree reclining position, when fed in the side-lying posture with head rotation to the left and the Mendelsohn maneuver, residue clearance was improved on the second VFSS on POD 34. The patient started taking gelatin jelly and continued swallowing exercises in side-lying with head rotation to the left and the Mendelsohn maneuver. With the same techniques, aspiration was not observed in the third VFSS on POD 50. We upgraded the patient’s diet to a pureed diet two months after surgery. The patient resumed taking a regular diet sitting upright by four months after the operations with no aspiration pneumonia.
CONCLUSION:
The use of side-lying posture, when combined with other techniques, has compensated for the unilateral pharyngeal dysmotility after cancer resection. This preliminary finding suggests that side-lying posture may be an option as a transitional compensatory technique for safe and effective swallowing until the patient returns to full oral intake.
1Introduction
Surgical resection of oropharyngeal cancer significantly alters oral and pharyngeal structures needed for swallowing and often results in dysphagia (Kao, 2016). When multiple swallowing-related structures are resected, swallowing impairment can become complex (Blyth, 2015). Physical exercises cannot restore structurally induced swallowing impairments fully. Thus, compensatory strategies, including postural changes (Logemann, 1994), diet and liquid texture modifications (Barbon, 2015), and swallowing maneuvers (Blyth, 2015), have been the basis of rehabilitative interventions for dysphagia after head and neck surgeries.
Various compensatory postures have been used to eliminate aspiration and improve bolus clearance by changing oral and pharyngeal dimensions and the direction of bolus flow (Logemann, 1994). Particularly, when the resection is limited in the unilateral side of the pharynx, the patient may be able to eat using his/her non-surgical side. For example, head rotation to the damaged side can eliminate the weak side from the bolus path and guide the bolus down the more functional side, thereby preventing pharyngeal residue and post-swallow aspiration (Logemann, 1994).
Side-lying can prevent post-swallow aspiration of the pharyngeal residue by accommodating the residue on the unilateral pharyngeal wall and the pyriform sinus until it is cleared with dry swallows (Lazarus, 2017). However, after early reports of side-lying (Logemann, 1994; Rasley, 1993), only one case study has described the application of this compensatory posture for a patient with severe dysphagia after traumatic brain injury (Drake, 1997). Thus, evidence to support the efficacy of this posture is lacking.
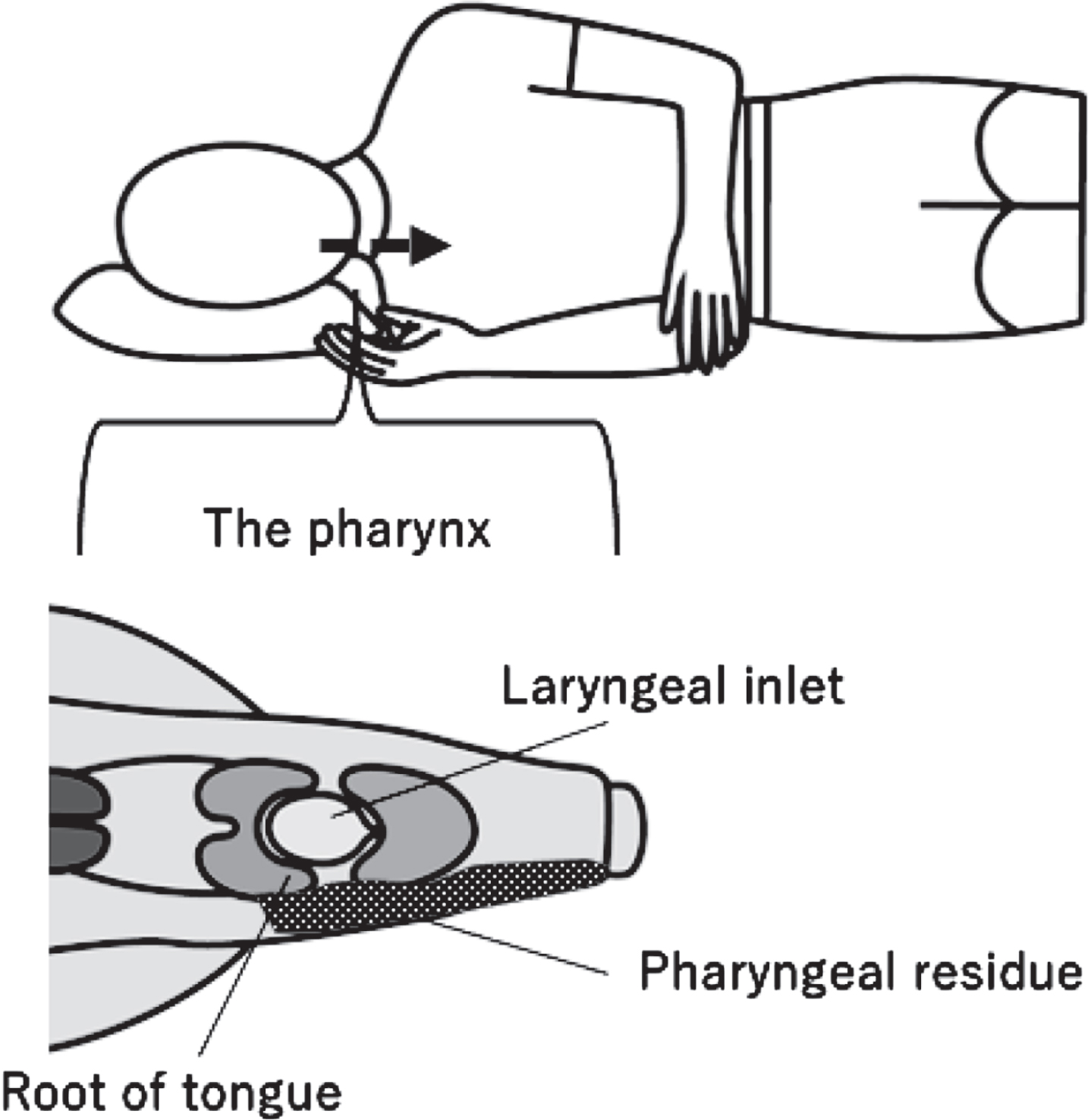
This case report aims to describe the utility of the side-lying posture in a patient with severe dysphagia after receiving multiple resections for left oropharyngeal cancer. We hypothesized that the side-lying posture could compensate for the unilateral pharyngeal dysmotility after cancer resection by guiding the bolus to the unaffected side of the pharynx and accommodating the residue until additional swallows could propel it entirely to the esophagus (Fig. 1).
Fig. 1
The side-lying posture. Bolus flows to the functional side of the pharynx (the dashed arrow) and can be held in the hypopharynx (the dotted area) without overflowing to the larynx. At the same time, the patient attempts to clear the residue with additional dry swallows.
2Patient information
This case study followed the CARE Guidelines (Gagnier, 2014) in reporting the patient. Written consent was obtained from the patient included in this report.
A 65-year-old male patient presented to our hospital with oropharyngeal carcinoma (pT2pN0pM0, Stage II) for surgical treatment in August 2020. The patient had a previous history of oral leukoplakia resections. Prior to the current hospital admission, he presented with tongue cancer and underwent partial surgical removal of the left oral tongue, the left floor of the mouth, and the left lateral pharyngeal wall in October 2019. He returned to a regular diet after these surgeries. In the current treatment, the patient underwent resections of the left tongue base and lateral pharyngeal wall with an anterolateral thigh flap reconstruction, left marginal mandibulectomy, partial left neck dissection (Level I-III), and tracheostomy. The attending otolaryngologist performed an endoscopic examination on postoperative day (POD) 7 and confirmed the flap with the normal color and vocal folds with normal mobility.
3Clinical findings
On POD 9, the patient was referred for swallowing assessment and rehabilitation. The patient presented with paralysis on the left lower lip, trismus, and limited movement of the left residual tongue. A cuffless tracheostomy tube with a speaking valve had been placed by the doctor’s decision. He was nil by mouth, receiving all nutrition via a nasogastric tube.
4Diagnostic assessment
On POD 10, otolaryngologists and the speech therapist jointly performed a videofluoroscopic swallowing study (VFSS). Contrast agent (Iohexol; Omnipaque, Daiichi Sankyo Co., Ltd. Tokyo, Japan) was delivered via a syringe, and the patient swallowed on command in each bolus trial. The Penetration-Aspiration Scale (PAS) (Rosenbek et al., 1996) scores were judged by a consensus of two otolaryngologists. The residue severity in the valleculae and pyriform sinuses was assessed using the Modified Barium Swallow Impairment Profile: MBSImPTM Component 16: Pharyngeal Residue (Martin-Harris, 2008).
A swallow of 5ml moderately thick liquid contrast agent (150–300 mPas) (Watanabe et al., 2018) in the head neutral position demonstrated severe dysphagia characterized by prolonged oral transit, reduced velopharyngeal closure, reduced tongue base retraction, incomplete contact of the tongue base to the posterior pharyngeal wall, premature spillage into the pharynx with delayed onset of swallowing, reduced pharyngeal contraction, reduced laryngeal elevation, and limited upper esophageal sphincter (UES) opening. The altered swallowing functions resulted in post-swallow aspiration (PAS score: 7) and severe pyriform sinus residue (MBSImP residue score 4; Fig. 2A).
Fig. 2
The initial videofluoroscopic swallowing study performed on POD 10. A: sit upright, neutral head position, 5ml moderately thick liquid swallow. B: sit upright, head rotation to the left, 5ml moderately thick liquid swallow. C: 45-degree reclining, head rotation to the left, 3ml moderately thick liquid swallow. Dashed arrows: pyriform sinus residue. Solid arrows: post-swallow penetration/aspiration.
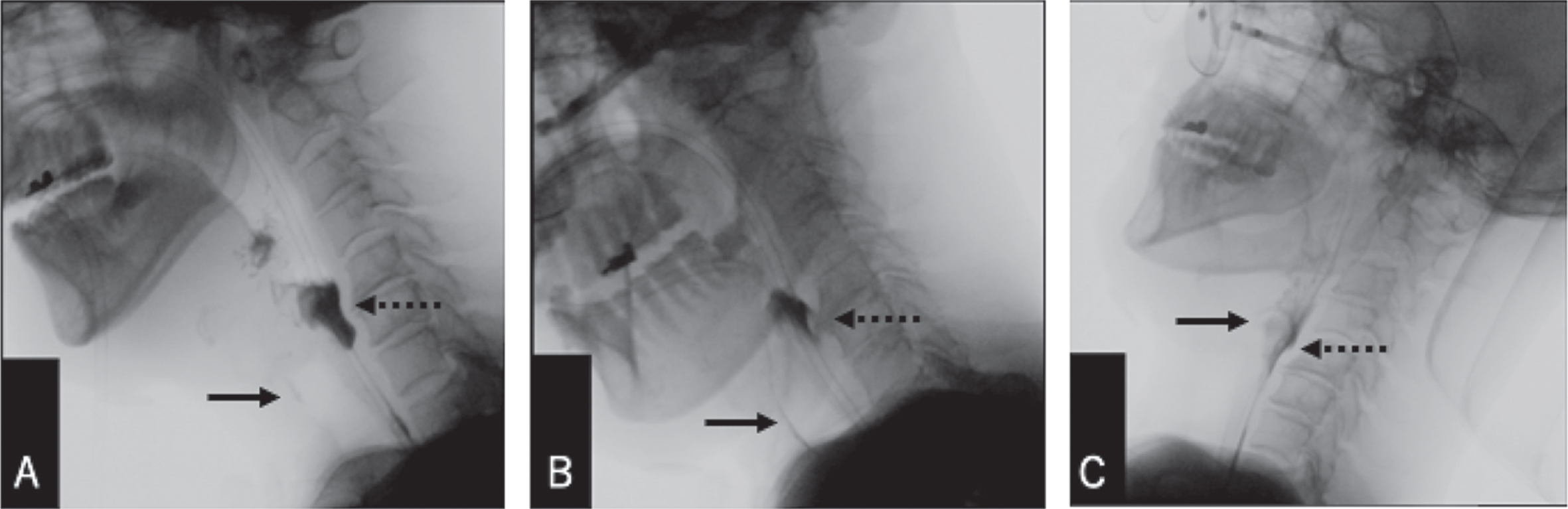
Additional dry swallows in the head neutral position did not help pharyngeal clearance. Head rotation to the damaged side (i.e., to the left) (Logemann, 1994) (Fig. 2B) on the initial bolus swallowing did not prevent aspiration (PAS score: 7) or improve pharyngeal clearance (MBSImP residue score: 4). When the patient swallowed 3ml of moderately thick liquid with his head rotated to the left in the 45-degree reclining position to prevent the bolus from overflowing to the larynx (Umeda, 2011) (Fig. 2C), airway protection and pharyngeal residue improved (PAS score: 5; MBSImP residue score: 3). The patient could cough out the material in the laryngeal vestibule on command.
5Therapeutic interventions
The otolaryngologists and the speech therapist advised the patient to use these compensatory strategies to prevent post-swallow aspiration of residue. We also instructed the patient to perform rehabilitative exercises three times a day, seven days a week, to maintain the functions of the non-surgical (right) side of oral and pharyngeal structures. The exercises included neck stretching, jaw-opening exercises (Wada, 2012), tongue strengthening exercises (Hsiang, 2019), the tongue-hold maneuver (Umeki, 2009), and the Mendelsohn maneuver (Doeltgen et al., 2017). The patient continued the exercises under the instruction of the speech therapist throughout his hospital stay.
On POD 11, with his speech therapist, the patient started taking moderately thick liquid in 45-degree reclining. He rotated his head to the left, adding multiple dry swallows and cough after the swallow. However, the patient needed more than 10-20 dry swallows until he cleared the bolus. After consuming a few spoons of liquid, he had to cough out the residue accumulated in the pharynx. Wet vocal quality and reflexive cough were observed after the swallow. Oral intake with the swallowing techniques was suspended for three days due to aspiration pneumonia that developed three days after restarting thickened liquids.
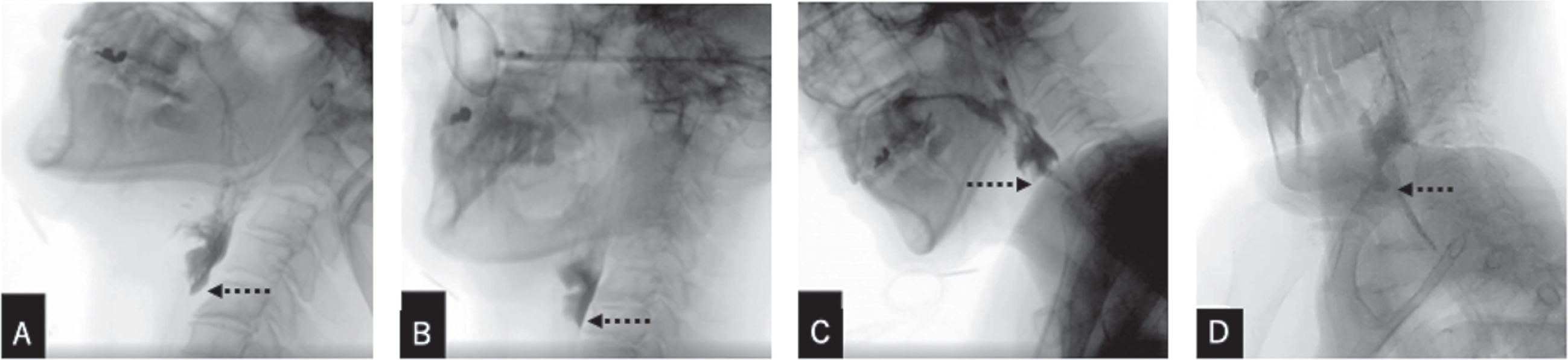
On POD 34, the second VFSS was performed to explore more effective compensatory strategies for better bolus clearance. The patient swallowed 3ml moderately thick liquid with the Mendelsohn maneuver throughout the VFSS trials as he had adopted it as his usual swallowing pattern. In the 45-degree reclining posture with a head neutral position, the patient demonstrated post-swallow aspiration (PAS score: 6) (Fig. 3A). Additional swallows with head rotation to the left (Fig. 3B) did not improve pharyngeal clearance. We then tested the side-lying posture. In the side-lying posture with the head neutral position (Fig. 3C), penetration and pyriform sinus residue remained (PAS score: 5; MBSImP residue score:4). Additional swallows did not help clear the residue. However, when fed in the side-lying posture with head rotation to the left and the Mendelsohn maneuver, residue was removed with few additional swallows (Fig. 3D). Thus, we advised the patient to continue swallowing exercises in side-lying with head turn to the left. We continued to monitor the effectiveness of the side-lying posture with VFSS.
Fig. 3
The 2nd videofluoroscopic swallowing study performed on POD 34, showing 3ml moderately thick liquid swallows using the Mendelsohn maneuver. A: 45-degree reclining, neutral head position. B: 45-degree reclining, head rotation to the left. C: Side-lying, neutral head position. D: Side-lying, head rotation to the left. Dashed arrows: Pyriform sinus residue clearance at the level of the UES.
6Timeline
Table 1 displays a timeline of swallowing assessment and rehabilitative intervention the patient underwent for two months. The table included the PAS scores and the MBSImP residue score in 3ml of moderately thick liquid swallows in the 45-degree reclining head neutral position in a series of VFSS to demonstrate longitudinal changes in the patient’s dysphagic symptoms.
Table 1
Swallowing assessment and rehabilitation
| Postoperative day | 1 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | |
| Treatment | PEG | RT | |||||||||||||||
| Assessment | VESS | ✓ | ✓ | ||||||||||||||
| VFSS (45° reclinmg, 3ml, moderately thick liquid) | ✓ | ✓ | ✓ | ✓ | |||||||||||||
| PAS score | 5 | 6 | 5 | 6 | |||||||||||||
| MBSImP score: vallecula residue | 1 | 1 | 1 | 1 | |||||||||||||
| MBSImP score: pyriform sinus residue | 4 | 4 | 3 | 4 | |||||||||||||
| Rehabilitation | Non-swalowing exercises | ||||||||||||||||
| Diet modification | gelatin jelly | pureed diet | |||||||||||||||
| Liquid modification | moderately thick | ||||||||||||||||
| Bolus size | 3ml | ||||||||||||||||
| Posture (body) | 45° reclining | side-lying | 30° side-lying | 45° reclining | |||||||||||||
| Posture (head) | head rotation to the left | ||||||||||||||||
| Swallowing techniques | multiple swallows, the Mendelsohn maneuver | ||||||||||||||||
| Outcome | Functional Oral Intale Scale (FOIS) | 1 | 2 | 3 | |||||||||||||
VESS: Videoendoscopic Swallowing Study. VFSS: Videofluoroscopic Swallowing Study. PEG: Percutaneous Endoscopic Gastrostomy, RT: Radiation Therapy. PAS: The Penetration-Aspiration Scale (1, no entry of material into the larynx or trachea; 8, material enters the trachea with no attempt to clear) (Rosenbek et al., 1996). The MBSImP: component 16 - Pharyngeal Residue (0 = Complete pharyngeal clearance, 4 = Minimal to no pharyngeal clearance) (Martin-Harris, 2008). FOIS: The Functional Oral Intake Scale (Crary, 2005).
In brief, the PAS scores and the MBSImP residue scores were stable throughout the rehabilitation period, suggesting that the swallowing impairment did not improve over time. However, with the various compensatory strategies listed in Table 1, the patient’s functional outcome scored by the 7-point Functional Oral Intake Scale (FOIS) (Crary, 2005) gradually increased from Level 1 (nothing by mouth) to Level 3 (tube dependent with consistent oral intake of food or liquid).
7Follow-up and outcomes
On POD 35, The patient started taking gelatin jelly in the side-lying posture with head turn to the left and the Mendelsohn maneuver (Fig. 4). The patient was also instructed to cough to eject the potentially aspirated/penetrated materials after each swallow. The number of dry swallows needed to clear a spoonful of jelly gradually decreased, and the total time to consume a cup of gelatin jelly shortened over time.
Fig. 4
Swallowing exercises in the right side-lying posture with left head rotation.

On POD 50, a third VFSS was repeated. In the 45-degree reclining posture with the neutral head position, the patient still presented with severe pyriform sinus residue and post-swallow penetration. However, in the right side-lying posture with head rotation to the left, penetration/aspiration was not observed with thin, mildly thick, and moderately thick liquids. The residue was cleared with multiple swallows.
On POD 53, the patient started taking half-portion pureed meals once a day in the side-lying posture with head rotation to the left. On POD 64, the patient started taking half-portion pureed meals three times a day in side-lying with a 30-degree tilt with the head rotation to the left to gradually return his posture to sitting upright during meals. On POD 67, he started taking half-portion pureed meals three times a day, seated upright with his head in the neutral position by his own decision despite the medical team’s recommendation to continue the side-lying posture. On the same day, the tracheostomy tube was removed. He also began receiving adjuvant radiation therapy (66 Gy) on POD 70.
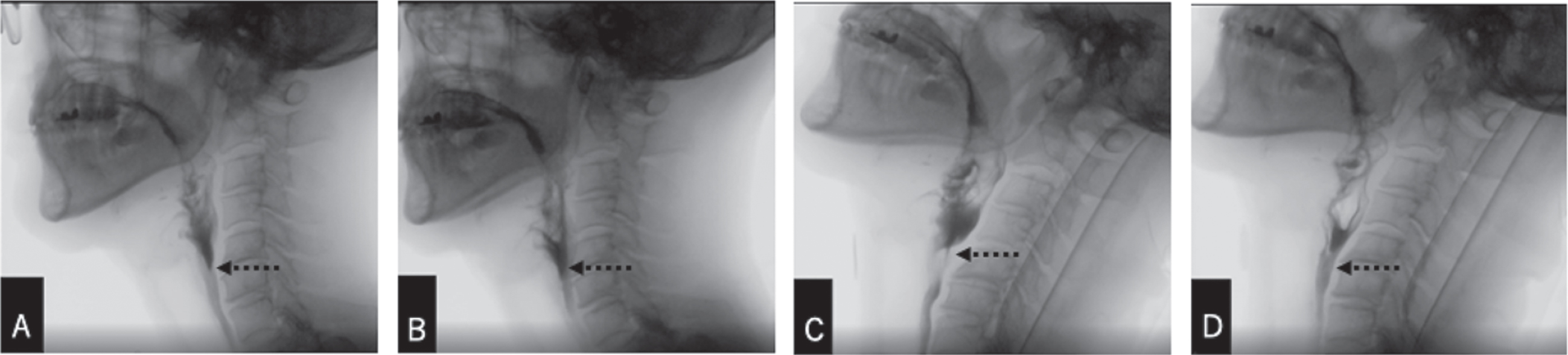
On POD 73, the final VFSS was performed to determine the diet and fluid recommendations for discharge. The Mendelsohn maneuver had already been his acquired swallowing pattern. The VFSS confirmed post-swallow silent aspiration and severe pyriform sinus residue on thickened and thin liquids in the upright and 45-degree reclining positions with the neutral head position. However, residue clearance with additional swallows became effective in all positions and with all consistencies (Fig. 5A-D). The patient’s voluntary cough ejected the aspirated materials. As described above, the patient had already restarted taking meals seated upright by his own decision. Therefore, we discussed options with the patient and suggested that he continue taking pureed meals and moderately thickened fluids in the 45-degree reclining posture with regular voluntary coughs to eject the potentially inhaled materials. On POD 75, the patient was discharged home. At four months post-operation, the patient had returned to a regular diet with no event of aspiration pneumonia.
Fig. 5
The 4th VFSS performed on POD 73. The patient employed the Mendelsohn maneuver across postures. A: sit upright, neutral head position; 3ml moderately thick liquid. B: sit upright, neutral head position; 3ml thin liquid. C: 45-degree reclining, neutral head position; 3ml moderately thick liquid. D: 45-degree reclining, neutral head position; 3ml thin liquid. Dashed arrows: The bolus passage to the esophagus with multiple dry swallows.
8Patient perspective
On POD 35, the patient reported that he required less effort to clear the pharyngeal residue with the side-lying posture. On POD 67, he said that he did not feel any residue after the swallow when he took meals seated upright. This favorable subjective judgment made him start taking meals without lying on the side by his own decision, although the medical team recommended continuing side-lying posture based on the VFSS findings.
9Discussion
Patients undergoing oral and oropharyngeal cancer resections exhibit multi-factorial swallowing dysfunctions. For example, resection of the oral tongue impairs bolus formation and transport, leading to prolonged oral transit time and oral residue. Tongue base resection results in pre-swallow spillage and pharyngeal residue. Excision of the soft palate or maxilla may result in nasopharyngeal regurgitation. A mandibulectomy impacts mastication significantly. Laryngeal elevation can be limited when suprahyoid muscles are resected, resulting in pyriform sinus residue and post-swallow aspiration (Borggreven, 2007).
The patient reported in this study presented with severe dysphagia after multiple surgeries for recurrent oropharyngeal cancer. In the absence of major postoperative complications such as flap failure, pain, or excess edema in the operating regions, the repeated extensive resections of the oral and pharyngeal structures may have been the main cause of the patient’s swallowing impairment.
Compensatory strategies have been the standard for managing irreversible dysphagia after cancer surgeries (Lazarus, 2017). The patient was educated to use the Mendelsohn maneuver to facilitate bolus clearance by increasing laryngeal elevation 19 and pharyngeal pressure 16. The patient also used head rotation to the damaged side to assist UES opening by reducing UES pressure (Takasaki, 2010) and increasing UES relaxation duration (Balou et al., 2014) of the undamaged side. A 45-degree reclining position was also used to allow the bolus to flow along the posterior pharyngeal wall without overflowing to the larynx by placing the respiratory tract in a superior position relative to the digestive tract (Umeda, 2011). However, these compensatory techniques did not mitigate the severe pyriform sinus residue and post-swallow aspiration, leading us to examine the effect of the side-lying posture.
To our knowledge, this is the first longitudinal observation on the use of the side-lying posture for achieving safe and efficient oral intake after head and neck cancer surgery. In this patient, when head rotation or the Mendelsohn maneuver did not help poor bolus clearance or post-swallow aspiration, adding side-lying led to effective bolus clearance with additional swallows. By lying on the unaffected side, the patient utilized the gravitational force to guide the bolus to the lower, unaffected side in the pharynx (Lazarus, 2017) This posture also accommodated more residue than the upright position in the right hypopharynx. These benefits allowed the patient with limited UES opening to prevent post-swallow aspiration by clearing residue held in the functional side of the hypopharynx.
It should be noted that two months of swallowing therapy did not improve the patient’s PAS scores or MBSImP residue scores over time. However, there was an increase in FOIS scores in the absence of functional improvements. These findings suggest that the side-lying posture can be a transitional compensatory technique for safe and effective swallowing until the patient returns to full oral intake.
The major limitation of the side-lying posture is that eating meals lying on the side is very uncommon, preventing patients with dysphagia from socializing through eating and limiting their quality of life. Therefore, it is essential to examine the effectiveness of less aggressive compensatory methods with repeated VFSS as the rehabilitation progresses. Additionally, gastroesophageal reflux may present an increased risk of aspiration when eating lying on the side.
The patient underestimated his swallowing impairment during meals and was unaware of persistent dysphagia identified in the final VFSS. This discrepancy between the patient’s subjective judgment of his swallowing function and the results of the objective swallowing assessment emphasizes the importance of VFSS to determine the effectiveness and risk of compensatory strategies for safe and efficient oral intake.
There are several limitations in this study. As this is a clinical case report, some variables could not be controlled. First, side-lying posture was not trialed until POD 34, although other techniques were trialed at POD 10. This was because of our clinical decision to start with less aggressive compensatory strategies. Second, along with side-lying, strategies such as head rotation and the Mendelsohn maneuver were used. Therefore, it was not possible to examine the effectiveness of side-lying alone, separating from the other strategies. However, it was confirmed that head rotation and the Mendelsohn maneuver together did not help bolus passage through the UES. Still, once the side-lying posture was added, residue was cleared with additional swallows. With these findings, it can be assumed that the side-lying posture could contribute to compensating for unilateral pharyngeal dysmotility after cancer resection by accommodating the residue in the unaffected side of the pharynx until additional swallows could propel it entirely to the esophagus. Third, observer bias was inevitable as the investigators of this case study were involved in the patient’s treatment. Prior knowledge of the patient’s treatment information may have influenced how data was collected, measured, or interpreted. However, the investigators used clear operational definitions in grading swallowing functions, aiming to minimize observer bias. Despite all the limitations, this case report can contribute to the literature providing detailed swallowing patterns in side-lying posture observed in the VFSS with a longitudinal follow-up.
Further research is warranted to investigate the effect of side-lying alone in a longitudinal study. Along with the functional outcomes, assessing the patient’s perception of swallowing and quality of life may be beneficial. For generalizability, the potential benefit of the side-lying posture should be tested in multiple patients with unilateral pharyngeal dysmotility after cancer resection and results should be reported in a case series.
10Conclusion
The use of side-lying posture, when combined with other techniques, may have compensated for the unilateral pharyngeal dysmotility after cancer resection. Side-lying posture may be an option as a transitional compensatory technique for safe and effective swallowing until the patient returns to full oral intake. The preliminary findings of this single case report will guide future research to examine the potential benefit of the side-lying posture.
Acknowledgments
The authors would like to acknowledge Melody Lo, M.S., CCC-SLP, for editing this paper. The authors would also like to thank Ayako Yoshimura for illustrating the figure.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1 | Balou, M , McCullough, G. H , Aduli, F , Brown, D , Stack, B. C Jr , Snoddy P , Guidry, T. ((2014) ). Manometric measures of head rotation and chin tuck in healthy participants. Dysphagia 29: (1), 25–32. https://10.1007/s00455-013-9472-y |
2 | Barbon, C. E. A. ((2015) ). Efficacy of thickened liquids for eliminating aspiration in head and neck cancer: a systematic review. Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery 152: (2), 211–218. |
3 | Blyth, K. M. ((2015) ). Speech and swallow rehabilitation following partial glossectomy: a systematic review. International Journal of Speech Language Pathology 17: (4), 401–410. |
4 | Borggreven, P. A. ((2007) ). Swallowing after major surgery of the oral cavity or oropharynx: a prospective and longitudinal assessment of patients treated by microvascular soft tissue reconstruction. Head & Neck 29: (7), 638–647. |
5 | Crary, M. A. ((2005) ). Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Archives of Physical Medicine and Rehabilitation 86: (8), 1516–1520. |
6 | Doeltgen, S. H , Ong, E , Scholten, I , Cock, C , Omari, T. ((2017) ). Biomechanical Quantification of Mendelsohn Maneuver and Effortful Swallowing on Pharyngoesophageal Function. Otolaryngology-Head and Neck Surgery 157: (5), 816–823 https://10.1177/0194599817708173. |
7 | Drake, W. ((1997) ). Eating in side-lying facilitates rehabilitation in neurogenic dysphagia. Brain Injury 11: (2), 137–142. |
8 | Gagnier, J. J. ((2014) ). The CARE guidelines: consensus-based clinical case report guideline development. Journal of Clinical Epidemiology 67: (1), 46–51. |
9 | Hsiang, C. ((2019) ). Early Postoperative Oral Exercise Improves Swallowing Function Among Patients With Oral Cavity Cancer: A Randomized Controlled Trial. Ear, Nose, & Throat Journal 98: (6), E73–E80. |
10 | Kao, S. S. ((2016) ). Swallowing outcomes following primary surgical resection and primary free flap reconstruction for oral and oropharyngeal squamous cell carcinomas: A systematic review. The Laryngoscope 126: (7), 1572–1580. |
11 | Lazarus, C. L. ((2017) ). History of the Use and Impact of Compensatory Strategies in Management of Swallowing Disorders. Dysphagia 32: (1), 3–10. |
12 | Logemann, J. A. ((1989) ). The benefit of head rotation on pharyngoesophageal dysphagia. Archives of Physical Medicine and Rehabilitation 70: (10), 767–771. |
13 | Logemann, J. A. ((1994) ). Effects of postural change on aspiration in head and neck surgical patients. Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery 110: (2), 222–227. |
14 | Martin-Harris, B. ((2008) ). MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia 23: (4), 392–405. |
15 | Rasley, A. ((1993) ). Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. American Journal of Roentgenology (1976) 160: (5), 1005–1009. |
16 | Rosenbek, J. C , Robbins, J. A , Roecker, E. B , Coyle, J. L , Wood, J. L. ((1996) ). A penetration-aspiration scale. Dysphagia 11: (2), 93–98. |
17 | Takasaki, K. ((2010) ). Influence of head rotation on upper esophageal sphincter pressure evaluated by high-resolution manometry system. Otolaryngology–Head and Neck Surgery 142: (2), 214–217. |
18 | Umeda, Y. ((2011) ). Effect of the reclining position in patients after oral tumor surgery. Journal of Medical and Dental Sciences 58: (2), 69–77. |
19 | Umeki, H. ((2009) ). Effects of a tongue-holding maneuver during swallowing evaluated by high-resolution manometry. Otolaryngology–Head and Neck Surgery 141: (1), 119–122. |
20 | Wada, S. ((2012) ). Jaw-opening exercise for insufficient opening of upper esophageal sphincter. Archives of Physical Medicine and Rehabilitation 93: (11), 1995–1999. |
21 | Watanabe, E , Yamagata, Y , Fujitani, J , Fujishima, I , Takahashi, K , Uyama, R , Ogoshi, H , Kojo, A , Maeda, H , Ueda, K , Kayashita, J. ((2018) ). The Criteria of Thickened Liquid for Dysphagia Management in Japan. Dysphagia 33: (1), 26–32. https://10.1007/s00455-017-9827-x |




