Non-modifiable worker and workplace risk factors contributing to workplace absence: A stakeholder-centred synthesis of systematic reviews
Abstract
BACKGROUND:
Workplace stakeholders report the identification and translation of relevant high quality research to inform workplace disability policy and practice is a challenge. The present study engaged academic and community stakeholders in conducting a best evidence-synthesis to identify non-modifiable risk and protective worker and workplace factors impacting work-related absence across a variety of health conditions.
OBJECTIVE:
To identify non-modifiable worker and workplace disability risk and protective factors impacting work-related absence across common health conditions.
METHODS:
The research team searched Medline, Embase, CINAHL, The Cochrane Library, PsycINFO, BusinessSource-Complete, and ABI/Inform from 2000 to 2011. Quantitative, qualitative, or mixed methods systematic reviews of work-focused population were considered for inclusion. Two or more reviewers independently reviewed articles for inclusion and methodological screening.
RESULTS:
The search strategy, including expert input and grey literature, led to the identification of 2,467 unique records. From this initial search, 2325 were eliminated by title or abstract review, 142 articles underwent comprehensive review to assess for inclusion, 26 systematic reviews met eligibility criteria for this synthesis. For non-modifiable worker and workplace factors we found consistent evidence across two or more health conditions for increased risk of disability in situations where workers experience lower education, older age, emotional distress, poor personal functioning, decreased physical functioning, psychological symptoms, overweight status, and greater sick leave history.
LIMITATIONS:
Heterogeneity of existing literature due to differences in outcome measures, definitions and research designs limited ability to assess effect size and results reflect findings limited to English-language papers.
1Introduction
Workers, employers, and society experience a significant burden due to workplace absence, prolonged disability, and related costs that accompany workers presenting with common chronic disease and injuries [1–3]. Research indicates a rising prevalence of chronic disability in the population [4, 5] and this increase in disability has been related to an increase in both direct and indirect costs. Direct costs involve aspects such as lost-time wage replacement, health care provider expenses, investigative tests, hospitalizations, surgeries, and disability settlements and pensions. Indirect costs may include loss of work productivity [6, 7], training of replacement workers, lost tax revenues, administrative expenses, as well as negative consequences for coworkers, supervisors and families [2, 8]. Specifically, workers and families often experience lost wages, suffering, pain, limited activities, and impacts on future employability [5].
Given substantial human and financial costs of workplace disability, ongoing research intended to assist in reduction of workplace illness and disability is warranted. However, even in cases when adequate research exists, full application of such knowledge may be limited. That is, in our work with stakeholders, a common difficulty voiced by these partners was their own lack of knowledge about how to identify high quality research, and subsequently, how to translate available best-evidence research into useful information intended to inform policy, training and practice [9–16]. Despite their motivation to learn from current research, stakeholders often found the literature challenging to translate into practical solutions that could be meaningfully applied within the workplace. Further, they reported that they lacked access to relevant research articles and that, even when they could identify and access appropriate articles, they required expert assistance in critical evaluation, including assessing scientific merit [9].
In addition to lack of access and interpretability of available research, workplace-based stakeholders also reported a lack of integration of knowledge concerning risk factors for work absences. Research is often focused on specific illnesses or disabilities, and stakeholders were concerned with the lack of comparison across health conditions. Stakeholders were particularly interested in the development of evidence-informed policies and principles relevant across a variety of common health conditions that could be made use of when targeting disability prevention. They were also interested in learning whether the findings were applicable to small or medium size employers who may not have disability managers or other dedicated human resources and, therefore, broad-spectrum guidance for prevention of disability was desired.
In order to help address these identified issues of access and translation, as well as to benefit from the knowledge and expertise of both workplace practitioners and researchers, we created an academic-community partnership (ACP) intent on addressing workplace disability prevention. An important purpose of our ACP was to provide primary knowledge users the opportunity to determine the value of the resulting data, while at the same time providing opportunity for researchers to ensure the integrity and quality of the resulting information. In this study, workplace practitioners were included as full research partners with equal input and direction over all components of the study. Given that typically workplace practitioners have been participants in research rather than full research partners, this aspect of our research plan provided both a novel and crucial component. With this approach, workplace stakeholders were able to establish boundaries for data translation, highlight concerns regarding data usefulness, provide feedback about workplace application, and help with data interpretation and synthesis as well as preparation of a summary relevant for stakeholders.
Our ACP was comprised of researchers from different fields and disciplines at three British Columbia, Canada (BC) universities, in collaboration with three community partners. The community partners comprised expertise from two occupational health andsafety organizations, and a not-for-profit health and welfare trust that provides group health and welfare benefits for over 100,000 employees in the health care and social service sector in BC. It is of note that success resulting from ACPs as a tool for facilitating knowledge-to-action (K2A) has been mixed in the literature [17–21]. In particular, questions about the scientific merit and societal value of ACPs have been raised as a result of research revealing that these collaborations often suffer from complicated definitional, conceptual, methodological, and translational issues [22–25]. In light of these difficulties, the present ACP characterized roles, responsibilities and key tasks, and created specific workflows to systematize the identification, prioritization and translation of high quality research. By utilizing an iterative problem identification and clarification process, the ACP discussions led to a decision to conduct a stakeholder-centered best-evidence synthesis of systematic reviews with the purpose of identifying disability risk and protective factors associated with work-related and chronic disease health conditions impacting work-related absences and disability duration.
This article reports findings of a subset of a larger ACP-directed search strategy identifying risk and preventive factors that impact work absence across health conditions and injuries. The present paper reports specifically on non-modifiable worker and work factors contributing to workplace absence. In previous articles, we reported on modifiable worker [26] and modifiable workplace [27] risk and protective factors and provided supplementary information related to the larger study.
2Methods
2.1Partnership process
Workplace stakeholders and academic researchers participated in defining the purpose of the systematic review via an organized and iterative process that employed face-to-face meetings, webconferencing, and use of minutes as “working documents.” This involved the circulation of draft minutes with instructions to the ACP team to use the minutes to provide further input and discussion. This provided an open space for both academic researchers and stakeholders who were absent from a given meeting to contribute to the discussion, as well as for those attending to provide further input following active reflection and additional input. Ideas were collated and circulated as part of a working document for discussion at the following meeting. This process was used during discussions regarding defining and refining the synthesis purpose as well as throughout the synthesis review process.
Stakeholders participated in the identification and refinement of keywords for the search parameters as well as the refinement of inclusion and exclusion criteria. An initial list of keywords was prepared by academic researchers and an information resource librarian. Stakeholders were invited to add additional keywords. We then conducted a series of pilot searches based on these keywords and provided stakeholders with a sample of literature retrieved. This initial ACP process led to refinement of the research question, expanded the list of search terms used in relevant studies, and resulted in the refinement of a set of stakeholder-centered inclusion/exclusion criterion used to inform the final search strategy. A minimum of two external librarians with expertise in health sciences, social sciences, and business databases, reviewed MeSH terms (structure language for Medline) and participated in its translation across search terms and parameters unique to each database being searched. A third librarian was used for final review.
2.2Stakeholder-centred inclusion/exclusion criteria
Based on discussions with stakeholders, inclusion criteria comprised of systematic reviews that included adults (age 15+) and a work-focused population (i.e. employed or attempting to secure employment). Systematic reviews that utilized quantitative (including meta-analysis) or qualitative syntheses were considered for inclusion. Systematic reviews were required to address risk or predictive factors for work absence outcomes related to employee personal illness or health condition(s), including physical and/or mental conditions. After piloting the search terms, exclusion criteria were expanded to exclude systematic reviews where the primary illness was a severe physical, mental and/or extremely rare condition, or reviews that focused on a specific special occupation such as air traffic controllers or police. Also excluded were systematic reviewsfocusing only on interventions with no discussion of risk or protective factors.
2.3Search strategies
An information specialist wrote all initial search strategies, with review by one or more selected peers. Search results were uploaded to RefWorks and then exported to Excel. Duplicates were removed manually.Alternate record sources included scoping searches, expert input, grey literature searches of health-evidence.ca, Rehab+, National Rehabilitation Infor-mation Center (NARIC), and Institute of Work and Health (IWH). Hand-searching of proceedings from a relevant conference (found in the EMBASE search) was also conducted. Following review of the initial search results, a second information resource officer reviewed and modified the search strategy as required, ensuring congruency with search terms. A copy of the search strategy is available upon request.
2.4Evaluation of quality and relevance
Evaluation for methodological quality of eligible studies used principles and procedures congruent with recommendations discussed in The PRISMA Statement and the Institute of Medicine’s Standards for Systematic Reviews [28]. This included (i) involvement of multiple information resource people, researchers and stakeholders in the development of search strategy, (ii) pilot-testing search strategy to characterize stakeholder-relevance of articles and search terms used in relevant retrieved articles, (iii) validation testing to assess the comprehensiveness of Medline search strategy, (iv) assessment of retrieved titles and abstracts for relevance, (v) selection of articles for further investigation, (vi) obtaining full text copies of these potentially eligible reviews, and assessing these reviews for relevance and quality (using independent assessment by at least two members of the review team), (vii) pilot testing abstraction process (for relevance and comprehensiveness) with stakeholders, and (viii) attention to production of final report relevant to stakeholders’ needs and organizational context.
The initial methodological criteria utilized an existing quality assessment tool for the groundwork. The tool employed was developed by researchers at McMaster University responsible for the development and maintenance of a website called ‘HealthEvidence.org’ supporting knowledge translation relevant to public health nursing. The original criteria was then compared with the EBM Glasgow Checklist for Systematic Reviews by researchers and assessed for congruency with AMSTAR methodological quality recommendations for critical appraisal of systematic reviews [29]. The ACP then reviewed and refined the methodological criteria using a process of sharing (email distribution), discussion, reflection and consensus. Changes were made in scoring and questions to improve the congruence of questions across different types (quantitative, qualitative or mixed) of systematic reviews (see Table 1).
The following questions/issues were asked of reviewers during the scientific review process: usefulness to small employers, research strengths/weaknesses, utilization suggestions from reviewers, and consistency with inclusion/exclusion criteria. A set of preliminary data abstraction formats were prepared by the research associate, and after review and modification by two researchers, were circulated to ACP members. After initial deliberations with stakeholders, the ACP created an abstraction form, and had a research associate abstract data from 10 potentially relevant articles. Stakeholders were then asked to select two or more articles and to highlight findings of interest and data abstracted from the research assistant. Stakeholders were also asked to reflect on additional abstraction categories that arose during this activity. Using this initial process as a guide, it was decided to add a category regarding applicability of the findings to small/ medium size businesses, and additional category to capture implementation guidance, if provided. Stakeholders were then requested to reconsider the initial categorization of factors once the abstraction tables were 90% complete. After extensive dialogue and agreement, this reassessment led to significant changes in the placement and naming of psychosocial and mental health factors. Following final agreement of factors, abstraction of the data into table format was completed and the table data was translated into meaningful factor-level messages as presented below. The present article addresses non-modifiable worker and workplace factors only.
3Results
3.1Search results
There were 2,467 unique records identified from all sources. Two or more researchers participated in an independent review process to cull articles that were not relevant to this synthesis, first by reviewing titles for all citations retrieved from the search. Citations were eliminated if both reviewers indicated the title gave sufficient information to eliminate it. All references remaining underwent a similar culling process assessing the title and abstract. This process led to the elimination of 2325 citations. If there was a disagreement between two researchers it was included for comprehensive review of the full article. This led to 142 articles being retrieved for comprehensive review to assess for inclusion. There were 26 systematic reviews that addressed non-modifiable worker and workplace factors included in this report. As shown in Table 2, the 26 studies that met the synthesis inclusion criteria varied considerably in sample characteristics and size, data sources, and outcome measures.
3.2Methodological quality results
The highest methodological score possible was 13 with a range of scores between 7 and 13 (these scores were subsequently translated into percentages). Fourteen studies were considered higher methodological quality systematic reviews (greater or equal to 85% ), three were considered medium quality reviews (between 75% – 84% ), and nine were considered lower quality reviews (between 50 – 74% ). All 26 systematic reviews were deemed to be of sufficient quality to contribute to evidence synthesis, with some of the lower quality scores resulting from limitations regarding the quality of primary studies informing the respectivesynthesis.
To assess inter-rater reliability, methodological results were downloaded into MS Excel from Fluid Surveys, with responses re-coded to reflect the scoring system employed. Kappa statistics were used to calculate the chance-adjusted between-reviewer agreement and disagreements per item and number of responses between sets of reviewers. This was calculated using an online kappa calculator (http://justusrandolph.net/kappa/). The overall inter-rater reliability score for the synthesis of the full set of 36 articles for the larger study was (0.752).
The studies included in the present analysis were heterogeneous in nature and therefore the use of a meta analytic statistical approach of combining data across systematic reviews to produce estimates of the effect was not possible. Best-evidence synthesis was therefore chosen to be our main method of critical appraisal [30, 31]. Best-evidence synthesis bases analysis on three aspects of evaluation: quality, quantity and consistency of available evidence [32]. For this best-evidence synthesis, the terms strong, moderate, and weak are not indicative of the predictive value of workplace factors. Rather, they are only a reflection of the consistency of evidence indicating whether a respective variable is a risk or protective factor across more than one health condition. Similarly, effect size or assessment of variance across reviews could not be determined given different outcome measures, types of studies, and level of reporting. Consequently, we used a team-developed framework created to indicate the consistency of a given factor in relationship to the methodological quality of the review (see Table 4). Importantly, this framework provided a method of adequately categorizing our evidence that fit well with the subjective perceptions of the team, and also offered a system through which all included reviews could be appropriately captured and described.
The ACP members also discussed the categorization of non-modifiable and modifiable factors, recognizing that the modifiability of some of these factors falls on a continuum from completely non-modifiable (e.g. age, length of employment, gender) to factors that are completely modifiable, such as offering appropriate work accommodation. For the purpose of this study, the research team classified worker and workplace factors that are less likely to be modified in the context of the workplace as non-modifiable factors. Under this rubric, factors considered to be less likely to be impacted at the workplace included enduring negative psychological characteristics (neuroticism), increased clinical and/or complicating factors, decreased physical functioning, and poor personal functioning. In the disability risk literature, there are also factors that could be changed in the future; however, the presence of such factors increases the risk of disability. These factors included the presence of emotional distress, psychological symptoms, respiratory conditions, or overweight status. The results section below comprises the complete list of worker and workplace factors considered to be non-modifiable within this classification.
3.3Evidentiary support for non-modifiable workplace factors
3.3.1Job level, general
Length of employment. One high-quality review found low evidence that, in cases of back and neck disorder, longer duration of employment decreased risk of sick leave of less than 3 months and of greater than 3 months [33]. Further, one low-quality review showed that for individuals suffering work-related back injuries, shorter employment periods were associated with poorer return to work outcomes [8]. Similarly, in cases of low back pain, lesser work tenure (newly hired) was associated with longer duration disability [34]. There is weak evidence that longer length of employment should be considered a predictor of work disability.
Job Grade. One moderate-quality review reported that low job grade was associated with a deceased likelihood of return to work for those experiencing mental illness or mental health conditions [35]. There is insufficient evidence that lower job grade should be considered a predictor of return to work.
Occupation. Occupation as a predictor of work disability and return to work was examined in four systematic reviews. In terms of increased work disability, one high-quality review that did not specify occupational levels showed strong evidence (more than 50% of studies agree) that occupation type was a predictor of work disability and lack of return to work for workers with rheumatoid arthritis. Further, these authors also demonstrated moderate evidence (25–50% of studies agree) of a similar relationship for workers with asthma or workers with ischemic heart disease [36]. A single low-quality review demonstrated moderate evidence (6 out of 9 studies) that blue collar or heavy manual work (versus white collar work) was a predictor for low back pain [34]. In relation to return to work, one high-quality review showed occupation (not specified) to be associated with reduced work resumption after myocardial infarction [37], and one-low quality review of construction workers found work-related injuries to be associated with poor return to work outcomes [8]. There is moderate evidence that lower occupational level should be considered a predictor for workdisability.
3.3.2Organizational level
Organizational economic and financial context. One high-quality review demonstrated organizational economic and financial context to be associated with the reduced likelihood of return to work for workers experiencing musculoskeletal and pain-related injury [38]. There is insufficient evidence that organizational economic and financial context should be considered a predictor of work disability.
Company size. Three high-quality reviews showed insufficient evidence of company size as a predictor of sick leave risk and becoming unemployed or changing jobs. One review reported that, in cases of psychosocial health concerns, companies greater than 100 employeeswere associated with increased risk of sick leave of more than 3 days [39]. In contrast, in cases of neck and back disorders, there was low evidence of increased risk of sick leave of less than 3 months for medium to large companies [33]. A single review showed that for companies less than 50 employees, respiratory conditions (including asthma) were associated with becoming unemployed or changing jobs [40]. There is inconsistent evidence that company size should be considered a predictor of work disability.
3.3.3Compensation and insurance level
Compensation level. One moderate-quality review showed low compensation level to be associated with increased risk of sickness absence related to psychological ill health [41]. Two low-quality reviews reported mixed findings. In one review both low and high compensation levels were associated with poor return to work outcomes in situations of work related back injury [8]. In a separate study, strong evidence linked high compensation level with decreased likelihood of return to work in cases of low back pain [42]. There is inconsistent evidence that compensation at high and low levels should be considered a predictor for work disability.
Loss of Benefits or Financial Disincentives to Work. A single low-quality review showed, for workers with spinal cord injury, loss of benefits or financialdisincentives to work were associated with a decreased likelihood of return to work [43]. There is insufficient evidence that loss of benefits or financial disincentives to work should be considered a predictor of return to work.
Workers Compensation Claim. Two high-quality reviews reported low evidence that work injury sickness benefits for low back pain were associated with increased risk of sick leave of less than 3 months [33]. Further, Peters et al. [40] found that filing of a workers’ compensation claim was associated with becoming unemployed or changing jobs in situations of asthma or respiratory conditions. There is moderate evidence that existence of a workers’ compensation claim should be considered a predictor of work disability.
Unemployment. A single moderate-quality review found that for workers with mental health conditions, the threat of unemployment was associated with a decreased likelihood of return to work, while re-employment within 6 months was predictive of a decline in depressive symptoms [35]. In a low-quality review, the unemployment rate was associated with poorer return to work outcomes resulting from work-related injury [8]. There is insufficient evidence that unstable employment should be considered a predictor of work disability.
3.3.4Healthcare system factors
A single moderate-quality review found that, for workers with low back pain, increased process-of-care quality significantly predicted reduced time off work and working status at three months [42]. There is insufficient evidence that healthcare systems factors should be considered a predictor of work disability.
3.4Evidentiary support for non-modifiable worker factors
3.4.1Sociodemographic
Dependents/Economic Condition. Only a single, lower-quality review addressing disability predictors and dependents, economic condition, and household income was found. This single study looking at workers with any health condition found that increased risk of poor Work Ability Index (WAI) score was predicted by the presence of underage children, decreased economic situation, and being the sole family wage-earner [44]. An additional high-quality review [36] provided weak evidence that higher socioeconomic status predicted lesser risk of work disability for workers with ischemic heart disease. There is insufficient evidence that having dependents, having a poorer economic situation, and/or being the sole wage-earner are risk factors for work disability.
Marital Status. Three systematic reviews considered marital status as a predictor for work disability. One review was high-quality [39], one moderate-quality [35], and one low-quality [43]. All reviews reported that being married was associated with an increased return to work for workers with psychosocial health conditions, mental health conditions and spinal cord injuries, respectively. There is moderate evidence that not being married or in a committed relationship should be considered a predictor for work disability.
Education. Ten systematic reviews considered education as a predictor of work disability. Only three high-quality reviews reported a robust relationship between education level and work disability. Specifically, De Croon et al. [45] reported strong evidence of lower education as a predictor for increased risk of work disability. Duijts et al. [39] found that lower education was associated with an increased risk of sick leave lasting more than 3 days (OR = 1.85). Detaille et al.[36] found moderate evidence of higher education as a predictor of reduced risk of work disability for individuals with rheumatoid arthritis. This was reported as a strong relationship for workers with ischemic heart disease.
Five reviews reported an association between level of education and work disability, but did not directly quantify the strength of the association. Three of these reviews were deemed to be of high quality.O’Neil et al. [37] found that education level was associated with reduced work resumption after myocardial infarction. Peters et al. [40] reported that for workers with respiratory conditions lower education was associated with being or becoming unemployed, as well as with job instability. One moderate-quality review [35] and two lower-quality reviews [8, 43] reported a lack of work experience as associated with a decrease return to work for respiratory and work-related injuries, respectively.
Finally, one high-quality review [46] regarding workers with depression and one low-quality review [44] regarding workers with any health condition reported weak and inconsistent associations respectively. Specifically, Lagerveld et al. [46] reported limited evidence that higher education predicted increased likelihood of better work participation outcomes, including return to work and work status. van den Berg et al. [44] found that lower education predicted increased risk of poor Work Ability Index (WAI) in one of only two studies. There is strong evidence that lower educational level should be considered a predictor for disability risk.
Age. Age as a predictor for disability risk was commonly evaluated in presently available systematic reviews. Specifically, three available reviews provided strong evidence for age as a predictor of disability risk. Two of these three were deemed high-quality studies [36, 45] and one was deemed of moderate-quality [42]. Both high-quality studies reported strong evidence of increased risk of work disability for older workers with cardiovascular and/or rheumatoid conditions, and the moderate quality study reported that increased age was related to a decreased likelihood of return to work for workers with low back pain. In addition, a single high quality systematic review provided moderate evidence for increased risk of poor work participation outcomes for people with depression, including return to work and work status, as predicted from olderage [46].
Several systematic reviews provided weak, inconsistent and/or uncategorized evidence of a relationship between age and disability risk. Specifically, two high quality systematic reviews provided weak evidence of age as a predictor. Dekkers-Sanchez et al. [47] found weak evidence that older age predicted increased risk of long-term sick leave for sick-listed workers. Hanssonand Jensen [33] found low evidence that older agepredicted increased risk of sick leave for workers with back and neck disorders of greater than 3 months and/or of requiring a disability pension. One high quality review found that older age was associated with reduced work resumption after myocardial infarction [37]. One moderate-quality review [35] reported that olderworkers with mental health conditions were more likely to take long-term disability, while younger workers with similar conditions were more likely to terminate employment. Two lower-quality reviews that reported older age as associated with poor return to work outcomes for workers with work-related back pain and cancer; however, the grade of evidence was not specified [8, 48]. Finally, a lower quality systematic review considering age as a predictor for any health condition was provided by van den Berg et al. [44]. These authors reported an inconsistent relationship between increased age and disability risk. There is strong evidence that older age should be considered a predictor for disability risk.
Rural residence. Two systematic reviews considered rural residence as a predictor for work disability. One high-quality review [36] looking at workers with ischemic heart disease found moderate evidence of rural residence as a predictor for work disability. Similarly, one low-quality review [49] regarding home care health workers found limited evidence of rural residence as a predictor for work disability. There is weak evidence that rural residence should be considered a predictor for work disability.
Gender. Four systematic reviews considered gender as a predictor for work disability. One moderate-quality review reported strong evidence of female gender as associated with decreased likelihood of return to work for workers with low back pain (Pooled RR for 10-year increments = 1.18 [42]. One high-quality review provided moderate evidence of female gender as a predictor of work disability in workers with rheumatoid arthritis (it should be noted that RA is known to be more prominent in females). This relationship between gender and work disability was also found as a weak relationship for female workers with ischemic heart disease or asthma [36]. Two additional reviews provided evidence of association without a description of strength of relationship. The low-quality review was consistent with the bulk of available reviews and reported an association between male gender and increased likelihood for return to work [43]. In contrast, the moderate quality review suggested that male gender was associated with increased sickness absence [35]. There is moderate evidence that female gender should be noted that a single moderate quality mental health systematic review found male gender as associated with increased sickness absence.
Age at onset of injury. Two reviews considered age of injury onset as a predictor of work disability. One high-quality review found weak evidence that development of rheumatoid arthritis after age fifty was related to increased risk of work disability [36]. One low-quality review found weak evidence of increased disability when spinal cord injury occurred at younger ages [43]. There is inconsistent evidence that age of injury should be considered a predictor of work disability.
Ethnic origin. Three reviews considered ethnic origin as a predictor of work disability. Two high-quality reviews [36, 45] looking at rheumatoid arthritis and ischemic heart disease, and one low-quality review looking at spinal cord injury, found weak evidence to suggest that non-white status was associated with increased risk of work disability [43]. It is important to note that these authors identified that people of non-white ethnicity experienced discrimination in attempting to return to work and/or finding alternate employment. There is strong evidence to suggest that non-white status should be considered a predictor of work disability.
3.4.2Emotional distress and depression
Three high-quality studies considered the impact of emotional distress on work disability. De Croon et al. [45] found weak evidence of increased risk of work disability related to rheumatoid arthritis for individuals with emotional or psychological distress. Duijts et al. [39] reported that very difficult life events and burnout predicted increased sick leave of three days or less. Davey et al. [50] found that burnout and job stress were associated with increased risk of unplanned, short-term work absences. There is strong evidence that emotional distress should be considered a predictor of work disability.
3.4.3Personal functioning and social support
Six systematic reviews considered the impact of perceived family stress/social support on work disability. One moderate-quality review reported strong evidence that social isolation/dysfunction was related to decreased likelihood of return to work (Pooled RR = 2.13) [42]. One low-quality review also found strong evidence that adverse life events experienced near the time of occupational back injury predicted increased work disability [51]. Two high-quality reviews also suggested a similar relationship. Detaille et al. [36] found that more support from friends was weakly association with reduced work disability for workers with cardiac conditions. Lagerveld et al. [46] reported limited evidence that decreased social and behavioural functioning predicted risk of poor work participation outcomes, including return to work and work status for those with depression.
Two low-quality reviews also suggested a similar pattern of results. Specifically, van den Berg et al. [44] found that difficult life situations outside of work predicted poorer Work Ability Index (WAI) score. Shaw et al. [34] reported that a lack of personal problems outside of the workplace predicted increased work ability. There is strong evidence that poor personal functioning should be considered a predictor for work disability.
3.4.4Clinical and/or complicating factors
Eight systematic reviews considered the relationship between clinical and/or complicating factors and work disability. Only two studies reported strong or moderate-level evidence, the remainder of the reviews provided weak evidence, or evidence with no categorical descriptor. Steenstra et al. [42] provided a moderate-quality review demonstrating a strong relationship between radiating pain and decreased return to work (Pooled RR = 2.49). Detaille et al. [36] provided the single high-quality review that discussed moderate level evidence. These authors reported that chest pain related to myocardial infarction or ischemic heart disease was related to increased work disability. They also reported weak evidence that several other clinical factors of heart disease (e.g. presence of congestive heart failure) were related to increased work disability risk. Further, Detaille and colleagues [36] reported moderate level evidence (25–50% of studies agree) that the presence of diabetes increased work disability, and weak evidence (10–25% of studies agree) that rheumatoid arthritis increased work disability.
Two other high-quality reviews discussed the relationship between these variables, but reported weak associations or did not categorize the association. Specifically, O’Neil et al. [37] reported that recurrent cardiac events and/or arrhythmia were associated with reduced work resumption after myocardial infarction. Hansson and Jensen [33] discussed low evidence of increased risk of sick leave, less than three months, in the presence of clinical symptoms of back and neck disorders.
Four low-quality reviews also suggested a general relationship between clinical and/or complicating factors and work disability. Lidal et al. [43] found that increased activities of personal care after spinal cord injury and a lack of medical complications predicted an increase in return to work. Similarly, these authors found that injury severity, pressure ulcers, and urinary infections predicted decreased return to work. Shaw et al. [34] found that traumatic low back pain was associated with an increased risk of work disability, as compared to that found in cases of non-traumatic low back injury. Spelten et al. [48] reported that clinical factors associated with cancer predicted poorer work outcomes. Similarly, Turner et al. [8] found that comorbid symptoms such as leg pain or sciatica predicted poorer return to work outcomes. There is strong evidence that increased clinical and/or complicating factors should be considered a predictor for workdisability.
Rheumatoid Arthritis. A single high-quality systematic review considered the relationship between rheumatoid arthritis and work disability. Detaille et al. [36] found strong evidence that greater somatic complaints of arthritis predicted increased work disability. These authors also reported weak-moderate evidence (depending on specific symptom) that increased clinical symptoms of arthritis predicted work disability. There is insufficient evidence that rheumatoid arthritis should be considered a predictor for work disability.
Functional Ability. Four systematic reviews considered the relationship between functional movement and work disability. Truchon et al. [52] provided a high-quality review that reported that decreased functional capacity predicted increased risk for work absence in cases of low back pain. O’Neill et al. (2010) also provided a high-quality review. The latter authors found that improvement in functional class predicted reduced work resumption after myocardial infarction. Turner et al. [8] provided a low-quality review linking decreased physical functioning scores with increased risk for work absence. Likewise, van den Berg et al. [44] provide a low-quality review linking musculoskeletal capacity (4 out of 4 studies) and functional balance (1 out of 2 studies) with increased risk of poor WAI scores. There is strong evidence that decreased physical functioning should be considered a predictor for work disability.
3.4.5Psychological symptoms
Twelve systematic reviews considered the relationship between psychological symptoms and work disability. One high-quality review discussed strong evidence (more than 50% of studies agree) of depression diagnosis or more somatic complaints as predictors of work disability for people with ischemic heart disease [36]. An additional high-quality review described moderate level evidence of comorbidity and/or Major Depressive Disorder (MDD) as associated with risk of disability [46].
Further, three high-quality and one moderate-quality reviews discussed associations between psychological symptoms and work disability, but did not categorize the degree of association. Specifically, Duijts et al. [39] reported that the presence of psychological symptoms was associated with increased risk of sick leave of 3 days or less (adjusted OR = 1.27) and of more than 3 days (adjusted OR = 1.97). Darr and Johns [53] discussed a relationship between psychological illness and increased risk of absenteeism. O’Neil et al. [37] reported that depression resulted in decreased work resumptions following myocardial infarction. Blank et al. [35] found that the presence of minor psychiatric disorder, phobia, and severity of mental health symptoms was associated with a decreased likelihood of return to work.
Two high-quality studies discussed weak relationships between specific psychological variables and work disability. Lagerveld et al. [46] found limited evidence that current or more frequent episodes of depression were related to risk of poor work participation outcomes. Detaille et al. [36] suggested weak evidence that more positive psychological scale scores predicted reduced risk of work disability for those with cardiac disease.
Finally, four low-quality reviews were available, each of which provided either weak evidence or uncategorized evidence of association. Specifically, Turner et al. [8] reported that for workers with work-related back pain, psychological distress was associated with poorer return to work outcomes. Fadyl et al. [51] found that psychological distress may lead to decreased work ability. Den Boer et al. [54] reported weak evidence that depression may be associated with reduced work capacity. Turner et al. [8] reported diagnosed personality disorder as associated with poor return to work outcomes. There is strong evidence that psychological symptoms should be considered a predictor for work disability.
3.4.6Enduring psychological characteristics
One high-quality and one low-quality systematic review considered the relationship between enduring psychological characteristics and work disability. Lagerveld et al. [46] provided a high-quality review that showed limited evidence of neuroticism as associated with poor work functioning outcomes, including productivity or performance at work. Fadyl et al. [51] provided a low-quality review that demonstrates a relationship between reduced cognitive performance and reduced work ability. There is weak evidence that enduring negative psychological characteristics should be considered a predictor for work disability.
3.4.7Respiratory conditions
Two high-quality systematic reviews considered the relationship between respiratory disorders and work disability. Detaille et al. [36] found weak evidence that asthma severity score was predictive of increased risk of work disability. Peters et al. [40] reported that diagnosed multiple chemical sensitivity was associated with slower return to being, or becoming employed, as well as to job instability. Peters et al. [40] also reported that chronic obstructive pulmonary disease or chronic non-specific lung disease was associated with slower return to work after work absence and that diagnosed asthma was related to several negative work outcomes. There is moderate evidence that presence of respiratory conditions should be considered a predictor for work disability.
3.4.8Weight
Six systematic reviews considered the relationship between weight and work disability. One high-quality study provided strong evidence that obesity was a predictor of long-term sick leave [55]. An additional high-quality review reported associations between being overweight and increased risk of sick leave of more than three days (crude OR [per SD BMI] = 1.54 [39]. Several moderate-quality articles provided similar conclusions. Specifically, Steenstra et al. [42] provided moderate evidence that being overweight was associated with decreased likely to return to work (Pooled RR = 1.68). Blank et al. [35] found that being overweight was associated with decreased return to work. These authors also reported that being underweight predicted a decrease in return to work.
Three low-quality studies also provided evidence of being overweight as a predictor for poorer work outcomes. Specifically, van den Berg et al. [44] found that poor WAI scores were associated with overweight status. Neovius et al. [56] reported that substantial weight loss in morbidly obese workers predicted a decrease in subsequent sick leave. There is strong evidence that overweight status should be considered a predictor for work disability.
3.4.9Intervention approaches
Time since treatment. A single low-quality systematic review considered the relationship between time since treatment and work disability. Spelten et al. [48] reported that greater time since treatment predicted more positive return to work outcomes. There is insufficient evidence that time since treatment should be considered a predictor for work disability.
Medication use. Two high-quality systematic reviews considered the relationship between medication use and work disability. Duijts et al. [39] reported that use of mental health medication was associated with increased risk of sick leave of three days or less (adjusted OR = 1.44) and of more than 3 days (adjusted OR = 3.13). Kuijer et al. [57] found limited evidence that the use of analgesics for low back pain increased risk of sickness absence at follow-up. There is weak evidence that medication use should be considered a predictor for work disability.
3.4.10Work injury, work status, length of employment, absence history
Work history. A single high-quality review considered the relationship between work history and work disability. Kuijer et al. [57] found limited evidence that in cases of chronic low back pain, having a current position or training environment was associated with less sickness absence at follow-up. There is insufficient evidence that work history should be considered a predictor for work disability.
Sick leave history. Five high-quality systematic reviews considered the relationship between sick leave history and work disability. Detaille et al. [36] found strong evidence that sick leave prior to operation was associated with increased risk of work disability for workers with ischemic heart disease. Lagerveld et al.[46] found moderate evidence that additional sick leave history predicted increased risk of poor work participation outcomes for workers with depression including return to work and work status. Dekkers-Sanche et al. [47] found weak evidence that sick leave greater than 100 days predicted increased risk of long-term sick leave. Hansson and Jensen [33] reported low evidence that sick leave history was related to increased risk of sick leave of less than 3 months (neck and back) and for less than 3 months and greater than 3 months (back only). Finally, Davey et al. [50] reported that for workers with mild illness or injury, greater sick leave history was associated with increased risk of unplanned short-term absences. There is strong evidence that greater sick leave history should be considered a predictor for work disability.
3.4.11Societal factors
A single low-quality systematic review considered the relationship between societal factors and workdisability. Lidal et al. [43] found that negative societal attitudes were associated with decreased risk of return to work for workers with spinal cord injuries. There is insufficient evidence that societal factors should be considered a predictor for work disability.
4Discussion
4.1Review of findings
For non-modifiable workplace factors, our synthesis only revealed lower occupational level as a factor with strong evidence as a predictor of disability. However, in addition to the variables with strong evidence, our synthesis indicated moderate level evidence that work disability could be predicted from existence of a workers’ compensation claim. For both the strong and moderate predictive factors, research was available across a wide variety of conditions (e.g., low back pain, rheumatoid arthritis, cardiovascular complaints etc.). However, all conditions investigated tended to be physiological in nature, limiting conclusions that could be drawn regarding the usefulness of these factors as predictors for psychosocial and/or psychological health.
In contrast to the non-modifiable workplace factors, but similar to the modifiable worker analysis, ample evidence was available with respect to systematic reviews for non-modifiable worker factors. For this analysis, strong evidence was available that increased work disability could be predicted from lower education, older age, non-white status (due to discrimination in the RTW process), emotional distress, poor personal functioning, increased clinical and/or complicating factors, decreased physical functioning, psychological symptoms, overweight status, and greater sick leave history. Also similar to the modifiable worker analysis, most of the non-modifiable worker factors appeared to be predictive of work disability across a wide variety of illnesses and/or injuries. Only two non-modifiable worker factors seemed to be less generalizable: non-white status and increased clinical and/or complicating factors. Specifically, for these two factors, available evidence seemed to primarily address physiological conditions.
With respect to non-modifiable worker factors with moderate evidence, non-married status, female gender, and presence of respiratory conditions were determined to be predictors of workplace disability. Of these factors, only female gender appeared to be consistently predictive across a variety of illnesses and injuries. In contrast, non-married status was demonstrated inrelation to mental health conditions and spinal cord injury, and presence of respiratory conditions was demonstrated only with respect to related respiratory illnesses.
4.2Implications and conclusions
With respect to non-modifiable workplace variables, our synthesis found few factors that may be useful for employers attempting to predict disability. Our synthesis found an increased risk of disability in situations where the respective injury is physiological and the worker experiences lower occupational level and/or existence of a workers’ compensation claim.
In contrast to few predictors at the workplace level, with respect to non-modifiable worker factors, our synthesis suggested that for employers attempting to predict disability, several factors should be considered as having strong and/or moderate level evidence for prediction across a variety of illnesses and/or disabilities. Specifically, our synthesis found that there is an increased risk of disability in situations where workers experience lower education, older age, emotional distress, poor personal functioning, decreased physical functioning, psychological symptoms, overweight status, and greater sick leave history.
Our synthesis also found that there is an increased risk of physiological disability in situations where workers experience non-white status (due to discrimination in the RTW process) and increased clinical and/or complicating factors.
4.3Limitations
There are several limitations in the present study and our results should be interpreted according to these limitations. Specifically, all reviews included in this research were written in English, potentially leading to some important non-English articles being missed. In addition, most systematic reviews were limited by the heterogeneity of existing literature due to differences in outcome measures, definitions and research designs. That is, our review is premised on the variance and quality of the reviews that came before us. Similarly, because we chose to include both quantitative and qualitative reviews in our best-evidence synthesis, we were unable to provide a quantitative summary of our conclusions.
Financial disclosure
This research was supported by a competitive research grant from WorkSafeBC through the Focus on Tomorrow program, and Healthcare Benefits Trust, a not-for-profit health and welfare trust. Neither grantor had any editorial control over manuscripts submitted for publication.
References
1 | Statistics Canada.Work Absence Rates. Ottawa, ON: Minister of Industry; 2011 May 1. Report No.: Catalogue no. 71-211-X |
2 | Health Canada. Economic Burden of Illness in Canada, 1998. Ottawa, ON: Minister of Public Works and Government Services Canada; 2002 |
3 | Health Council of Canada. Why Health Care RenewalMatters: Learning from Canadians with Chronic Health Conditions. Toronto, ON: Health Council of Canada; 2007 |
4 | Dewa CS, Lin E, Kooehoorn M, Goldner E (2007) Association of chronic work stress, psychiatric disorders, and chronic physical conditions with disability among workers Psychiatr Serv 58: 5 652 658 |
5 | Dewa CS, Lin E (2000) Chronic physical illness, psychiatric disorder and disability in the workplace Soc Sci Med 51: 1 41 50 |
6 | Schultz IZ, Gatchel RJ (2008) Research and Practice Directions in Risk for Disability Prediction and Early Intervention Handbook of Complex Occupational Disability Claims. Early identification, intervention and prevention Schultz IZ, Gatchel RJ 523 39 New York Springer |
7 | Melhorn JM, Lazarovic J, Roel WK (2008) Do we have a disability epidemic? Handbook of Complex Occupational Disability Claims. Early identification, intervention and prevention Schultz IZ, Gatchel RJ 7 24 New York Springer |
8 | Turner JA, Franklin G, Turk DC (2000) Predictors of chronic disability in injured workers: A systematic literature synthesis Am J Ind Med 38: 6 707 722 |
9 | White MI, Kube D, Petruniak J, Myette L, King L, Johnston R (2007) Best Practices Leadership Summit on Disability Prevention Vancouver, BC Canadian Institute for the Relief of Pain and Disability |
10 | White MI, Richman J, Kerr S, Toro Posada S (2004) Enhancing Stakeholders’ Knowledge and Skills in Disability Prevention, Detection and Management Vancouver, BC Canadian Institute for the Relief of Pain and Disability |
11 | Guzman J, Yassi A, Baril R, Loisel P (2008) Decreasing occupational injury and disability: The convergence of systems theory, knowledge transfer and action research Work 30: 3 229 239 |
12 | Loisel P, Durand MJ, Baril R, Gervais J, Falardeau M (2005) Interorganizational collaboration in occupational rehabilitation: Perceptions of an interdisciplinary rehabilitation team J Occup Rehabil 15: 4 581 590 |
13 | Franche RL, Baril R, Shaw W, Nicholas M, Loisel P (2005) Workplace-based return-to-work interventions: Optimizing the role of stakeholders in implementation and research J Occup Rehabil 15: 4 525 542 |
14 | Loisel P, Buchbinder R, Hazard R, Keller R, Scheel I, van TM (2005) Prevention of work disability due to musculoskeletal disorders: The challenge of implementing evidence J Occup Rehabil 15: 4 507 524 |
15 | Frank J, Cullen K (2006) Preventing injury, illness and disability at work Scand J Work Environ Health 32: 2 160 167 |
16 | Frank J, Sinclair S, Hogg-Johnson S, Shannon H, Bombardier C, Beaton D (1998) Preventing disability from work-related low-back pain New evidence gives new hope–if we can just get all the players onside. CMAJ 158: 12 1625 1631 |
17 | Townsend AL, Ishler KJ, Vargo EH, Shapiro BM, Pitorak EF, Matthews CR (2007) The FACES Project: An academic-community partnership to improve end-of-life care for families J Gerontol Soc Work 50: 1-2 7 20 |
18 | Ofili E, Igho-Pemu P, Lapu-Bula R, Quarshie A, Obialo C, Thomas C (2005) The Community Physicians’ Network (CPN): An academic-community partnership to eliminate healthcare disparities Ethn Dis 15: 4 Suppl 5 S5 S7 |
19 | Trauth JM, Jernigan J, Myers SM, Potter M, Fedor K, Procopio J (2003) Developing an academic-community partnership in the context of Pennsylvania’s State Health Improvement Plan Public Health Rep 118: 2 169 174 |
20 | Berkowitz B (2000) Collaboration for health improvement: Models for state, community, and academic partnerships J Public Health Manag Pract 6: 1 67 72 |
21 | Hall KL, Stokols D, Moser RP, Taylor BK, Thornquist MD, Nebeling LC (2008) The collaboration readiness of transdisciplinary research teams and centers findings from the National Cancer Institute’s TREC Year-One evaluation study Am J Prev Med 35: 2 Suppl S161 S172 |
22 | Stokols D, Hall KL, Taylor BK, Moser RP (2008) The science of team science: Overview of the field and introduction to the supplement Am J Prev Med 35: 2 Suppl S77 S89 |
23 | Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK (2008) Moving the science of team science forward: Collaboration and creativity Am J Prev Med 35: 2 Suppl S243 S249 |
24 | Masse LC, Moser RP, Stokols D, Taylor BK, Marcus SE, Morgan GD (2008) Measuring collaboration and transdisciplinary integration in team science Am J Prev Med 35: 2 Suppl S151 S160 |
25 | Feinberg ME, Bontempo DE, Greenberg MT (2008) Predictors and level of sustainability of community prevention coalitions Am J Prev Med 34: 6 495 501 |
26 | Wagner S, White M, Schultz I, Murray E, Bradley SM, Hsu V (2014) Modifiable worker risk factors contributing to workplace absence: A stakeholder-centred best-evidence synthesis of systematic reviews Work 49: 4 541 558 |
27 | White M, Wagner S, Schultz IZ, Murray E, Bradley SM, Hsu V Modifiable workplace risk factors contributing to workplace absence across health conditions: A stakeholder-centered best-evidence synthesis of systematic reviews Work 45: 4 1 12 |
28 | Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: Institute of Medicine of the National Academies; 11 A.D. Mar 23 |
29 | Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C (2007) Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews BMC Med Res Methodol 7: 10 |
30 | Slavin RE (1995) Best evidence synthesis: An intelligent alternative to meta-analysis J Clin Epidemiol 48: 1 9 18 |
31 | Carroll LJ, Cassidy JD, Peloso PM, Giles-Smith L, Cheng CS, Greenhalgh SW (2008) Methods for the best evidence synthesis on neck pain and its associated disorders: The Bone and Joint Decade -Task Force on Neck Pain and Its Associated Disorders Spine (Phila Pa 1976) 33: 4 Suppl S33 S38 |
32 | Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J (2005) Workplace-based return-to-work interventions: A systematic review of the quantitative literature J Occup Rehabil 15: 4 607 631 |
33 | Hansson T, Jensen I (2004) Swedish Council on Technology Assessment in Health Care (SBU). Chapter 6. Sickness absence due to back and neck disorders Scand J Public Health Suppl 63: 109 151 |
34 | Shaw WS, Pransky G, Fitzgerald TE (2001) Early prognosis for low back disability: Intervention strategies for health care providers Disabil Rehabil 23: 18 815 828 |
35 | Blank L, Peters J, Pickvance S, Wilford J, Macdonald E (2008) A systematic review of the factors which predict return to work for people suffering episodes of poor mental health J Occup Rehabil 18: 1 27 34 |
36 | Detaille SI, Heerkens YF, Engels JA, van der Gulden JW, van Dijk FJ (2009) Common prognostic factors of work disability among employees with a chronic somatic disease: A systematic review of cohort studies Scand J Work Environ Health 35: 4 261 281 |
37 | O’Neil A, Sanderson K, Oldenburg B (2010) Depression as a predictor of work resumption following myocardial infarction (MI): A review of recent research evidence Health Qual Life Outcomes 8: 95 |
38 | MacEachen E, Clarke J, Franche RL, Irvin E (2006) Systematic review of the qualitative literature on return to work after injury Scand J Work Environ Health 32: 4 257 269 |
39 | Duijts SF, Kant I, Swaen GM, van den Brandt PA, Zeegers MP (2007) A meta-analysis of observational studies identifies predictors of sickness absence J Clin Epidemiol 60: 11 1105 1115 |
40 | Peters J, Pickvance S, Wilford J, Macdonald E, Blank L (2007) Predictors of delayed return to work or job loss with respiratory ill-health: A systematic review J Occup Rehabil 17: 2 317 326 |
41 | Michie S, Williams S (2003) Reducing work related psychological ill health and sickness absence: A systematic literature review Occup Environ Med 60: 1 3 9 |
42 | Steenstra IA, Verbeek JH, Heymans MW, Bongers PM (2005) Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature Occup Environ Med 62: 12 851 860 |
43 | Lidal IB, Huynh TK, Biering-Sorensen F (2007) Return to work following spinal cord injury: A review Disabil Rehabil 29: 17 1341 1375 |
44 | van den Berg TI, Elders LA, de Zwart BC, Burdorf A (2009) The effects of work-related and individual factors on the Work Ability Index: A systematic review Occup Environ Med 66: 4 211 220 |
45 | De Croon EM, Sluiter JK, Nijssen TF, Dijkmans BA, Lankhorst GJ, Frings-Dresen MH (2004) Predictive factors of work disability in rheumatoid arthritis: A systematic literature review Ann Rheum Dis 63: 11 1362 1367 |
46 | Lagerveld SE, Bultmann U, Franche RL, van Dijk FJ, Vlasveld MC, van der Feltz-Cornelis CM (2010) Factors associated with work participation and work functioning in depressed workers: A systematic review J Occup Rehabil 20: 3 275 292 |
47 | Dekkers-Sanchez PM, Hoving JL, Sluiter JK, Frings-Dresen MH (2008) Factors associated with long-term sick leave in sick-listed employees: A systematic review Occup Environ Med 65: 3 153 157 |
48 | Spelten ER, Sprangers MA, Verbeek JH (2002) Factors reported to influence the return to work of cancer survivors: A literature review Psychooncology 11: 2 124 131 |
49 | Franche RL, Murray EJ, Ostry A, Ratner PA, Wagner SL, Harder HG (2010) Work disability prevention in rural healthcare workers Rural Remote Health 10: 4 1502 |
50 | Davey MM, Cummings G, Newburn-Cook CV, Lo EA (2009) Predictors of nurse absenteeism in hospitals: A systematic review J Nurs Manag 17: 3 312 330 |
51 | Fadyl JK, McPherson KM, Schluter PJ, Turner-Stokes L (2010) Factors contributing to work-ability for injured workers: Literature review and comparison with available measures Disabil Rehabil 32: 14 1173 1183 |
52 | Truchon M, Fillion L (2000) Biopsychosocial determinants of chronic disability and low-back pain: A review J Occup Rehabil 10: 2 117 142 |
53 | Darr W, Johns G (2008) Work strain, health, and absenteeism: A meta-analysis J Occup Health Psychol 13: 4 293 318 |
54 | den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW (2006) A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery Eur Spine J 15: 5 527 536 |
55 | van Duijvenbode DC, Hoozemans MJ, van Poppel MN, Proper KI (2009) The relationship between overweight and obesity, and sick leave: A systematic review Int J Obes (Lond) 33: 8 807 816 |
56 | Neovius K, Johansson K, Kark M, Neovius M (2009) Obesity status and sick leave: A systematic review Obes Rev 10: 1 17 27 |
57 | Kuijer W, Groothoff JW, Brouwer S, Geertzen JH, Dijkstra PU (2006) Prediction of sickness absence in patients with chronic low back pain: A systematic review J Occup Rehabil 16: 3 439 467 |
Figures and Tables
Fig.1
Results of search strategy PRISMA chart.
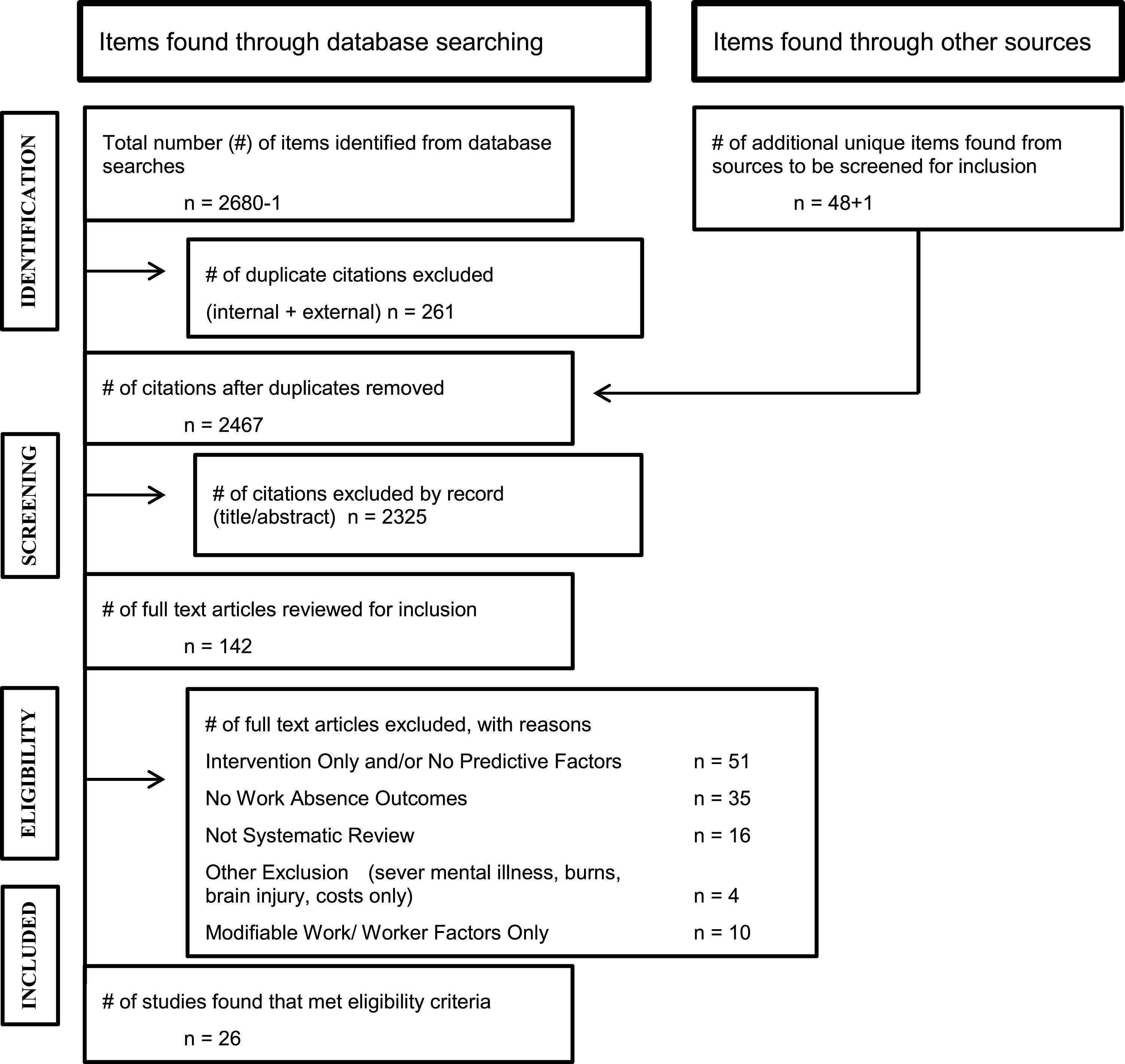
Table 1
Methodological quality review
| Common criteria for both qualitative and quantitative methodological review | ||
| Question | Answer choice | Score |
| Did the authors have a clearly focused question? | Yes | 1 |
| No | 0 | |
| Were inclusion/exclusion criteria used? | Yes | 1 |
| No | 0 | |
| Not specified | 0 | |
| Did the authors describe a search strategy | Yes | 1 |
| that was comprehensive and reproducible? | No | 0 |
| Not specified | 0 | |
| Please click the search strategies used | (selected/unselected) | a. Five or more databases: 2 |
| b. Two to four databases: 1 | ||
| c. One database: 0 | ||
| Did search strategy cover an adequate | Yes | 1 |
| number of years? (10+ years) | No | 0 |
| Does the data support the author’s interpretation? | Yes, mostly | 1 |
| No | 0 | |
| Are there any concerns related to COI? | Yes | 0 |
| No | 1 |
| Specific criteria quantitative methodological quality | ||
| Question | Answer choice | Score |
| Did the review assess the methodological | Yes | 1 |
| quality of the primary studies: | No | 0 |
| What methods did the authors use to combine or | Meta-analyses | 2 |
| compare results across studies? | Descriptive + quality weight | 2 |
| Descriptive no weight | 1 | |
| Other | 0 | |
| How strong was the level of evidence supporting the | Level 1 (RCT) | 2 |
| strongest conclusions of the study? | Level 2 (non-random) | 1 |
| Level 3 (uncontrolled) | 0 | |
| Unclear | 0 | |
| Total score possible: 13 |
| Specific criteria qualitative &mixed methodological quality | ||
| Did the review assess the methodological quality | Yes | 1 |
| of the primary studies? (minimum of 4) | ||
| □ suitability of methodology/paradigm to the research question | No | 0 |
| □ sampling (selection of participants/settings/documentation) | ||
| □ clear description of context, data collection, and data analysis | ||
| □ rigor (audit trail, some coding by 2 or more coders, | ||
| deviant case analysis, respondent validation) | ||
| □ triangulation | ||
| □ reflexivity (researcher and research process) | ||
| □ relevance (credibility, consistency, applicability, transferability) | ||
| Was this methodological quality review incorporated in the | Descriptive + quality weight | 2 |
| data analysis (weighting of higher quality studies)? | ||
| Descriptive no weight | 1 | |
| Other | 0 | |
| How strong was the level of evidence supporting the | Level 1 (RCT) | 2 |
| strongest conclusions of the study? | ||
| Level 2 (non-random) | 1 | |
| Level 3 (uncontrolled) | 0 | |
| Unclear | 0 | |
| Total score possible: 13 |
Table 2
Characteristics of studies included in synthesis
| Study citation | Number &type of studies included in review | Number of relevant studies | N Total and Range of N | Results: Populations included in reviewed studies |
| [35] Blank et al. J Occup Rehabil, 2008; 18:27–34. | 15 studies: 9 cohort, 5 retrospective interviews/ questionnaires | 15 studies. | N total = 21,617 Range of N = 95 to 10,308 | 5 studies on non-specified workers; 2 studies of civil servants; 2 studies of finance/ insurance workers; 1 study of contract workers; 1 study on mine workers; 1 study of supervisors; 1 study of recently unemployed; 1 study of teachers; 1 study of steel and automotive workers (blue collar); 1 study of student nurses. |
| [53] Darr &Johns. J Occup Health Psych, 2008; 13(4): 293–318. | 115 published studies and 22 dissertations. | 137 studies, total. | N total = N/A Range of N = Not provided | Occupations covered: Medical profession; manufacturing, production; social work; blue-collar workers; administration; government; retail; security-related fields. |
| [50] Davey et al. J Nurs Manag, 2009; 17:312–330. | 16 articles met inclusion and quality criteria – representing 14 studies: 7 prospective, 7 not prospective. | 16 | N total = 4,915 Range of N = 71 to 1107 | Hospital nurses |
| [45] De Croon et al. Ann Rheum Dis, 2004; 63:1362–1367. | 13 studies met inclusion criteria and were rated high or medium quality | 13 studies. | N total = Not provided Range of N = Not provided | Details of studies not provided. |
| [47] Dekkers-Sánchez et al. Occup Environ Med, 2008; 65:153–157. | 5 studies met the inclusion criteria: 4 of high quality, 1 of medium quality. | 5 studies. | Range of N = 328 to 3,628 N total = 5,731 | 1 study of municipal/ county employees; 1 study of profit and non-profit employees; 3 studies of general workers. |
| [54] den Boer et al. Eur J Spine, 2006; 15:527–536. | 11 studies | 4 use work capacity as an outcome. | Range of N = 46 to 177 N total = 332 (N not provided for 1 study) | Occupational characteristic not provided. |
| [36] Detaille et al. Scand J Work Environ Health, 2009; 35(4): 261–281. | 43 studies: 32 high quality; 11 medium quality. No studies for diabetes; Not enough studies for COPD to allow synthesis; 3 studies for asthma; 20 studies for rheumatoid arthritis; 21 studies for ischemic heart disease | 43 studies; all cohort studies. | N total = 15,883 Range of N = 25 to 633 | Occupational characteristic not provided. |
| [39] Duijts et al. J Clin Epidemiol, 2007; 60:1105–1115. | 20 articles: prospective cohort studies, in English, all except 1 from Europe. | 20 studies. | N total = Not provided. Range of N = Not provided. | 4 studies on non-specified employees; 3 studies on hospital/ health care staff; 2 studies on electricity firm employees; 2 studies on municipal employees; 2 studies on manufacturing employees; 2 studies on civil servants |
| 2 studies on industrial employees. 1 study on nurses; 1 study on truck drivers; 1 study on nurses’ aides | ||||
| [51] Fadyl et al. Disabil Rehabil, 2010; 32 (14): 1173–1183. | 23 articles met quality criteria. | 23 articles. | N total = Not provided Range of N = Not provided | Details of included studies not provided. |
| [49] Franche RL et al. Rural Remote Health, 2010; Oct-Dec;10(4):1502 Epub 2010 Oct 16 | 5 studies (3 cross-sectional – self-administered anonymous questionnaire, 1 cross-sectional &longitudinal), *workplace absence-cohort claims database | 1 study with work-related outcome. | N Total = 386 | home health care workers |
| [33] Hansson &Jensen. Scand J Public Health, 2004; 32:109–151. | 28 studies met inclusion criteria and were of sufficient quality | 28 studies | N total = Over 54,283 (one study includes all retail, construction, and manufacturing employees in Ontario, sample size not included). Range of N = 98 to 13,962 (at least, see comment above) | Occupations typically not reported. |
| [57] Kuijer et al. J Occup Rehabil, 2006; 16: 439–467. | 17 studies (28 papers): 4 prognostic cohort studies, 13 randomized controlled trials. | 17 studies. | N total = 2,046 Range of N = 49 to 253 | Details of occupational categories not provided. |
| [46] Lagerveld et al. J Occup Rehabil; 2010, 20:275–292. | 25 studies: 16 cross-sectional studies; 9 longitudinal studies. | 19 studies focused on work participation. 11 studies focused on work functioning. | Work participation: N total = 28,130 Range of N = 49 to 13,359 Work functioning: N total = 5,611 Range of N = 49 to 2,341 Overall N total: 29,703 | Work participation: 15 studies described as “non-specified groups of workers”; 2 studies with workers in finance and insurance industry; 1 study with workers in manufacturing; 1 study with workers in call centers. |
| Work functioning: | ||||
| 10 studies described as “non-specified groups of workers”; 1 study with workers in call centers. | ||||
| [43] Lidal et al. Disabil Rehabil, 2007; 29 (17): 1341–1375. | 123 studies. | 123 studies. | N total = 69,115 Range of N = 12 to 20,143 | Occupations not given. |
| [38] MacEachen et al. Scand J Work Environ Health, 2006; 32:257–269 | 13 qualitative studies met quality criteria | 13 studies. | Range of N = 10 to 85 N total = 513 | Occupations not described. |
| [41] Michie et al. Occup Environ Med, 2003; 60:3–9. | 49 studies met the inclusion criteria | 49 studies | N total = 99,716 Range of N = 26 to 15,530 | 22 studies of health care workers; 11 studies of general workers; 3 studies of office workers; 1 study of engineers; 1 study of blue collar workers; 1 study of police and firefighters; 1 study of white collar workers; 1 study of teachers |
| [56] Neovius et al. Obesity Rev, 2009; 10:17–27. | 36 studies: 32 non-interventions; 4 interventions. | 36 studies. | Details of sample sizes not provided. | Details of occupations not provided. |
| [37] O’Neil et al. Health Qual Life Outcome, 2010; 8:95. | 12 articles met inclusion criteria. | 12 articles | N total = 2795 Range of N = 88 to 620 | Employed at time of myocardial infarction, no occupational details. |
| [40] Peters, J. et al. J Occup Rehabil, 2007; 17(2): 317–26. | 5 studies met the inclusion criteria; 4 cohort studies and 1 observational study | 5 studies | N total = 797 Range of N = 55 to 251 | 4 studies of general worker; 1 study of mental workers and office clerks |
| [34] Shaw et al. Disabil Rehabil, 2001; 23 (18): 815–28. | 22 studies (7 Patient Survey, 6 – Claims Database+1 Chart Review/Claims Database, 1 Clinic Database/Claims Database 4 Physician Exam/Patient Survey, 2 Chart Review, 1 Physician Exam | 22 | Insured populations/ occupational health clinics | |
| [48] Spelten et al. Psycho-oncology, 2002; 11: 124–131. | 14 studies met the inclusion criteria. | 14 studies. | N total = 2,433 Range of N = 12 to 403 | Occupational categories not described. |
| [42] Steenstra et al. Occup Environ Med, 2005; 62:851–860. | 14 studies: 6 prospective; 8 retrospective | 14 | N total = 104,676 Range of N = 120 to 89,190 | 1 general population; 3 workers’ comp populations; 3 insurance settings; 2 occupational physician settings; 1 occupational setting; 1 orthopaedic clinic; 1 work injury database; 1 clinical setting. |
| [52] Truchon et al. J Occup Rehabil, 2000; 10(2): 117–142. | 18 studies met the inclusion criteria. | 18 studies. | N total = 23,290 Range of N = 78 to 11,762 | 10 studies of clinical populations; |
| 3 studies general worker populations; | ||||
| 2 studies of blue collar workers; | ||||
| 1 study of workers’ compensation registers; | ||||
| 1 study of military workers. | ||||
| [8] Turner et al. Am J Indust Med, 2000; 38:707–722. | 20 studies: 13 on low back injuries only, 7 on other injuries in addition to low back. | 20 studies. | N total = 85,285 Range of N = 47 to 25,093 | 10 studies of claimants; |
| 9 studies of workers with LBP; 1 study of nurses | ||||
| [44] van den Berg et al. Occup Environ Med, 2009; 66:211–220. | 20 studies: 14 cross-sectional and 6 longitudinal. | 20 studies. | Range of N = 88 to 5,622 N total = 18,747 | 4-non-specified workers; 6-municipal workers; 2-office workers; 2 studies on home care workers; 1-care givers; 1-firefighters; 1-metal and retail workers; 1-physicians. |
| [55] van Duijvenbode et al. Int J Obesity, 2009; 33:807–816. | 13 longitudinal studies | 13 studies | Range of N = 255 to 21,419 N total = 73,642 | 3 studies with non-specified workers; 2 studies with welders, metal workers and office clerks in construction; 3 studies with civil service workers; 2 studies with oil refinery workers; 1 study with industrial, administrative and service sector workers; 1 study with university employees; 1 study with nursing students; |
Table 3
Methodological quality review rating
| Ref # | Author | Year | Clearly focused question? | Inclusion/exclusion | Comprehensive | # of search strategies | # of years | Methodological quality | Methods weighting | Strength of evidence | Congruence data &author interpretation | COI | Quality Score |
| [35] | Blank, L. et al. | 2008 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 1 | 1 | 1 | 10 |
| [53] | Darr, W. et al. | 2008 | 1 | 1 | 1 | 2 | 1 | 0 | 2 | 1 | 1 | 1 | 11 |
| [50] | Davey, M.M. et al. | 2009 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| [45] | De Croon, E.M. et al. | 2004 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [47] | Dekkers-Sanchez, P.M. et al. | 2008 | 1 | 1 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 1 | 11 |
| [54] | Den Boer, J.J. et al. | 2006 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8 |
| [36] | Detaille,S. I. et al. | 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [39] | Dujits, S.F. et al. | 2007 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [51] | Fadyl, J.K. et al. | 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [49] | Franche, R.L. et al. | 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 9 |
| [33] | Hansson, T. et al. | 2004 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [57] | Kuijer, W. et al. | 2006 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 2 | 1 | 1 | 13 |
| [46] | Lagerveld, S.E. et al. | 2010 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [43] | Lidal, I.B. et al. | 2007 | 1 | 1 | 1 | 2 | 0 | 0 | 1 | 1 | 1 | 1 | 9 |
| [38] | MacEachen, E. et al. | 2006 | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
| [41] | Michie, S. et al. | 2003 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 10 |
| [56] | Neovius, K. et al. | 2009 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 7 |
| [37] | O’Neil, A. et al. | 2010 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | 12 |
| [40] | Peters, J. et al. | 2007 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| [34] | Shaw, W.S. et al. | 2001 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 8 |
| [48] | Spelten, E.R. et al. | 2002 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 8 |
| [42] | Steenstra, I.A. et al. | 2005 | 1 | 1 | 1 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 10 |
| [52] | Truchon, M. et al. | 2000 | 1 | 1 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 1 | 11 |
| [8] | Turner, J.A. et al. | 2000 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 8 |
| [44] | van den Berg, T.I. et al. | 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 9 |
| [55] | van Duijvenbode, D.C. et al. | 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 11 |
Table 4
Level of evidentiary support across systematic reviews
| Strong |
| •A minimum of 3 high-quality |
| •A minimum of 2 high-quality AND 2 moderate-quality or low-quality |
| •A minimum of 1 high-quality AND 3 or more of moderate-quality or low quality |
| Moderate |
| •A minimum of 2 high-quality |
| •A minimum of 1 high-quality AND 2 moderate-quality or low-quality |
| •A minimum of 4 moderate-quality or low-quality |
| Weak |
| •A minimum of 1 high-quality AND 1 moderate-quality or low-quality |
| •A minimum of 3 moderate-quality of low-quality |
| Inconsistent* |
| •The studies do not meet the criteria for any level of evidence and there |
| is no consistent agreement in reported outcomes. |
| Insufficient* |
| •Information is not inconsistent but does not meet the criteria for weak evidence |
*The focus of this synthesis was the identification of risk factors, not the impact of interventions on work absence. Due to diversity of both clinical and occupational interventions and respective integrative conclusions, a summary statement cannot be made and thus evidence is labeled “inconsistent.” However, factors identified in the included intervention studies may represent emerging or promising data for further investigation.
Table 5
Evidentiary support for non-modifiable workplace factors
| Strong | Moderate | Weak | Inconsistent | Insufficient |
| Lower occupational level [8, 34, 36, 37] | Longer length of employment [8, 33, 34] | Company size [33, 39, 40] | Lower job grade [35] | |
| Existence of a workers’ compensation claim [33, 40] | Compensation at high and low levels [8, 41, 42] | Loss of benefits or financial disincentives to work [38] | ||
| Unstable employment [8, 35] | ||||
| Healthcare systems factors [42] | ||||
| Negative societal factors [43] |
Table 6
Evidentiary support for non-modifiable worker factors
| Strong | Moderate | Weak | Inconsistent | Insufficient |
| Lower educational level [8, 35–37, 39] [40, 43] [44–46] | Not being married or in a committed relationship [35, 39, 43] | Rural residence [36, 49] | Age at onset of injury [36, 43] | Having dependents, having poorer economic situation, and/or being the sole wage-earner [36, 44] |
| Older age [8, 33, 35–37, 42, 44–48] | Female Gender [35, 36, 42, 43] | Enduring negative psychological characteristics [46, 51] | Rheumatoid arthritis [36] | |
| Non-white status [36, 43, 45] | Presence of respiratory conditions[36, 40] | Time since treatment [48] | ||
| Emotional distress [39, 45, 50] | Medication use [39, 57] | |||
| Poor personal functioning [34, 36, 42, 44] [46, 51] | ||||
| Increased clinical and/or complicating factors [8, 33, 34, 36] [37, 42, 43, 48] | ||||
| Decreased physical functioning [8, 37, 44, 52] | ||||
| Psychological symptoms [8, 35–37, 39, 46, 51, 53, 54] | ||||
| Overweight status [35, 39, 42, 44, 55, 56] | ||||
| Sick Leave history [33, 36, 46, 47, 50] |



