3D reconstruction images of cone beam computed tomography in dental medicine application: A case study and mini-review
Abstract
Dental cone beam computed tomography (CBCT) is a new approach in diagnosis and predication of various dental diseases, including trauma, congenital defects, tumors and inflammatory. In this study, we reported the outcome of CBCT for a complicated case of malocclusion, accompanied with tooth loss and periodontitis. A combined application of CBCT with 3D-static images and rotated reconstruction images is reviewed as a systematic model in diagnosis, treatment and progonsis of a complex malocclusion.
1Introduction
Malocclusion (i.e. poor bite) is an incorrect relation or misalignment between the teeth of the two dental arches when the jaws close. It is often involved in the causal dental and skeletal disharmonies. Malocclusion is one of the most common dental disorders in pediatric population. Its incidence in children is as high as 68% [1]. Malocclusion can be caused by various problems, such as genetic factors, cleft lip and palate, crowns or braces in unappropriated position, abnormally shaped or impacted teeth, tumors in the mouth or jaw, injuries that result in the misalignment, poor dental care, thumb sucking in the early childhood, prolonged usage of bottle feeding in the early childhood, frequent usage of pacifier after the age 3. The clinical manifestation of malocclusion are of several types, including the individual malposed tooth, the abnormality of dental arch and tooth arrangement, the abnormality of the relationship between dental arch, jaw, and facial tissues [2] (i.e. crowded teeth, crossbite, overbite, underbite, or open bite). Malocclusions may have influence on facial proportion, oral hygiene, maxillofacial function, and social and psychologic status.
The treatment methods for malocclusions include the preventive orthodontics, interceptive orthodontics, general orthodontics and combined orthodontic and surgical treatment [3]. Radiographs are an indispensable tool in dental clinical treatment, including the traditional radiographic method such as panoramic and lateral cephalograms, posterior bitewing radiographs and anterior periapical radiographs, traditional CT technology, 3D-static images and rotated reconstruction images generated by CBCT.
Intraoral, panoramic and cephalometric radiographs are the basic imaging techniques in dentomaxillofacial. But the effect of these radiographs was affected by exposure conditions, quality of photographic file, development process and so on.
The traditional CT technology also has 3D images, but its application is limited due to high radiation dosages, high cost, long hours for scanning, certain degree of deformation and artifacts of existing metal (i.e. metal ceramic crown or tooth filling materials), which might be affected by surrounding tissues of maxillofacial structures, especially alveolar bone.
CBCT has been widely used in diagnosis of the lesions in airway tract system [4, 5], root position and structure [6, 7], orthognathic surgical planning [8], temporomandibular joint evaluation [9], positions of impacted teeth [10, 11], evaluation of skeletal asymmetries [12, 13], and miniscrew placement [14, 15]. CBCT uses a lower radiation dose than traditional CT technology and results in a higher level of distinguishability and accuracy than is found with 2D images, such as cephalometry and panoramic radiographs [16]. The microstructure of dentoskeletal hard tissue can be seen with CBCT. The images have little distortion and artifact caused by metal might be observed [17]. The transaction of CBCT has no overlap image, which displays 3D morphology of the craniofacial skeleton, by virtual 3D reconstruction with a high degree of accuracy [18]. 3D-static images and rotated reconstruction images can be both generated by CBCT. 3D-static images can provide detailed information of a certain site, while 3D-rotated images can be rotated from every direction and the changes of teeth and dent skeletal changes in the treatment can be clearly observed [19].
Here, we reported a case of an adult malocclusion patient with loss of teeth and periodontitis. The impact of 3D-rotated images and static images generated by CBCT evaluation in diagnosis of complex malocclusion was discussed and a mini-review was made.
2Case report
A 33-year-old man came with the chief complaint of an unesthetic dental appearance. His maxillary right lateral incisor had been missing for several years ago due to trauma. The patient had received no treatment during that time, and he had no history of smoking or bad oral habits. Physical examinatin showed poor oral health, thick dental calculusbands, incisor protrusion and large gaps between the maxillary incisors. The gap between the maxillary incisors and the incisal protrusion had increased. His maxillary right lateral incisor was missing, and his maxillary left central incisor was extruded. Scattered space existed between the upper anterior teeth. He had a severe deep overjet (12.0 mm) and overbite (5.0 mm), and his mandibular central incisors slightly impinging the gingiva of the upper jaw. Occlusal trauma could be observed on the palatal mucosa. The available maxillary space was 11.0 mm, and the crowding degree of the mandible was 1.0 mm (Fig. 1.A).
The CBCT examinations were performed using a device with a flat panel detector (aSi) size of 20×25 cm (KaVo 3D exam; KaVo, Biberach, Germany) and reconstructed using i-CAT Vision software (Imaging Sciences International, Hatfield, Pa). A panoramic radiograph showed that all teeth were present except the maxillary right lateral incisor (Fig. 2.A). The mandibular left third molar was mesioangularly impacted. Extensive resorption of alveolar bone, primarily in the anterior regions, could be observed on the radiograph. The root resorption caused by trauma of the maxillary right central incisor could be observed by CBCT, which showed that palatal alveolar bone resorption was 1/3 of the root level of the maxillary left central incisor and the alveolar bone resorption was at the mid-root level of the mandible incisors (Fig. 3).
The treatment objectives were to achieve a stable occlusion, restore esthetics, function, and periodontal health in the anterior region, maintain the existing occlusion in the posterior region and replace the spaces between the incisors. Therefore, the complete periodontal therapy was perfomed to re-establish a stable occlusion, restore esthetics and function, prevent mutual aggravation of occlusal trauma and periodontitis, and create the space for prosthodontic treatment. These procedures prevented mutual aggravation of occlusal trauma and periodontitis, to attain better facial esthetics and restoration of the dentition defect.
Twenty-nine months after treatment, all brackets were removed. Thirty-one months after treatment, a free gingival graft (FGG) was performed to increase the thickness of the labial gingival, and a final restoration with a hybrid ceramic facing crown was then performed (Fig. 1.B). The occlusal trauma had been relieved, and the severe periodontitis was well controlled throughout the orthodontic treatment.
3Detailed information obtained by static images generated by CBCT
Newly formed trabecular bone could be observed on static images generated by CBCT in the maxillary and mandibular anterior regions, and the height of lingual bone plate was increased (Fig. 2.B, Fig. 3). No further root resorption was observed in the maxillary right central incisor.
4Overall perspective from 3D-rotated images
The pre- and post-treatment 3D-rotated images were created using Dolphin Software (version 11.0; Dolphin Imaging Systems, Chatsworth, Calif). They showed marked improvement of the anatomic morphology of the dentofacial region. The 3D images also showed that a normal overjet and overbite were established, a stable occlusion was achieved, and occlusion in the anterior region was improved (Fig. 4). The maxillary central incisors were corrected with proper intrusion and alignment.
5Discussion
Malocclusion often causes periodontal diseases and missing teeth [20]. Proper orthodontic treatment combined with periodontal treatment can achieve a better occlusion and prevent the aggravation of occlusal trauma and periodontitis [21].
In recent years, successful dental multidisciplinary therapy has required that problems be considered on an individual basis, and that with a comprehensive diagnosis and treatment plan be based on the knowledge and skills of all involved disciplines [22]. In this study, the patient’s periodontitis was obviously relieved, and a stable occlusion was achieved after treatment. Furthermore, post-treatment CBCT showed that a harmonious facial pattern was achieved, and newly formed alveolar bone was observed in some regions. A normal overjet and overbite were established that improved occlusion in the posterior region.
Radiographs are a commonly-used diagnosis tool in orthodontic treatment [23] . With the advent of CBCT, it is now possible for clinicians to evaluate the hard and soft tissues of the maxillofacial region in 3D and high spatial detail. CBCT utilizes a cone- or pyramid-shaped X-ray beam that is directed on the pursued maxillofacial field-of-view. PC Chien et al. suggested that CBCT allowed overall improved interobserver and intraobserver reliability in certain landmarks in vivo when compared with two-dimensional images [24]. The high accuracy of CBCT images is a valuable tool for analysis of tooth structure and adjacent anatomy [25]. The advantages and disadvantages of traditional 2D radiographs, traditional CT technology and CBCT are shown in Table 1.
There are various indications which cannot be adequately interpreted from 2D images or 3D-static images and therefore will benefit from 3D-rotated images. 3D reconstruction rotated images can be created by utilizing the original CBCT data using analysis software such as Dophin, In vivo, and Anatomage. They have certain advantages that other radiological technologies do not have. First of all, a large number of 2D X-ray pictures could be replaced by the 3D-rotated images as patient information could be observed different directions. Furthermore, it is beneficial for both clinicians and patients or their family members to have a better understanding of the patient’s pathogenic condition, which could improve the communication between doctors and patients. In addition, the availability of the 3D-rotated images significantly increases the confidence of orthodontists and helps them make better diagnosis and treatment plans, as the information obtained from the 3D-rotated images is more accurate than that obtained from traditional 2D images. Finally, by comparing the pre- and post-treatment 3D-rotated images, treatment results can be clearly and directly assessed. In this study, the occlusal relationship, the arch form and the midline could be observed from different directions. This information obtained from the CBCT scan could influence the patient’s final treatment outcome by helping clinicians develop a better diagnosis and treatment plan [26].
However, it should be reminded that the 3D-rotated images should not necessarily replace the static images, as the specific information of each tooth and its alveolar bone, root position and shape can not be measured. As the 3D-rotated images can only present general information for clinicians, it is essential for orthodontists to combine 3D-static images and rotated reconstruction images when diagnosing, treating and evaluating patients.
6Conclusions
Dental CBCT has its unique advantage in evaluation of the hard and soft tissues of the maxillofacial region in high spatial resolution. The 3D-rotated images are fasion for overall evaluation of a patient and doctor-patient comunication, while the 3D-static images generated by CBCT can display the specific status of a certain site (i.e. root position and structure, positions of impacted teeth, the quality and quantity of alveolar bone and so on). We propose that a combination of 3D-static images and rotated reconstruction images generated by CBCT can be used in diagnosis of complex malocclusion cases, which aids improving the prognosis and treatment of dental disorders.
Acknowledgments
This research was supported by The National Natural Science Foundation of China (No. 81570981), and The Chongqing Research Program of Basic Research and Frontier Technology (No. cstc2014jcyjA10039).
References
[1] | Minkui F. , Ding Z. , Bangkang W. et al., The prevalence of malocclusion in China: An investigation of 2 children, Chin J Stomatol 37: ((2002) ), 371–373. |
[2] | Angle E.H. , Treatment of malocclusion of the teeth: Angle’s system: White Dental Manufacturing Company, (1907) . |
[3] | Graber T.M. , Orthodontics: Principles & Practice: WB Saunders Company, (1972) . |
[4] | Tso H.H. , Lee J.S. , Huang J.C. , Maki K. , Hatcher D. and Miller A.J. , Evaluation of the human airway using cone-beam computerized tomography, Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 108: ((2009) ), 768–776. |
[5] | El H. and Palomo J.M. , Measuring the airway in 3 dimensions: A reliability and accuracy study, American Journal of Orthodontics and Dentofacial Orthopedics 137.4: ((2010) ), 121–124. |
[6] | Lund H. , Gröndahl K. and Gröndahl H.-G. , Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment, Angle Orthodontist 80: ((2010) ), 466–473. |
[7] | Makedonas D. , Lund H. , Gröndahl K. and Hansen K. , Root resorption diagnosed with cone beam computed tomography after 6 months of orthodontic treatment with fixed appliance and the relation to risk factors, The Angle Orthodontist 82: ((2011) ), 196–201. |
[8] | Swennen G.R. , Mollemans W. , De Clercq C. , et al., A cone-beam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning, Journal of Craniofacial Surgery 20: ((2009) ), 297–307. |
[9] | Motta A.T.Sd. , Carvalho Fd.A.R. , Oliveira A.E.F. , Cevidanes L.H.S. and Almeida M.Ad.O. , Superimposition of 3D cone-beam CT models in orthognathic surgery, Dental Press Journal of Orthodontics 15: ((2010) ), 39–41. |
[10] | Guerrero M. , Shahbazian M. , Elsiena Bekkering G. , Nackaerts O., Jacobs R. and Horner K., The diagnostic efficacy of cone beam CT for impacted teeth and associated features: A systematic review, Journal of Oral Rehabilitation 38: ((2011) ), 208–216. |
[11] | Bjerklin K. and Ericson S. , How a computerized tomography examination changed the treatment plans of 80 children with retained and ectopically positioned maxillary canines, The Angle Orthodontist 76: ((2006) ), 43–51. |
[12] | AlHadidi A. , Cevidanes L. , Mol A. , Ludlow J. and Styner M. , Comparison of two methods for quantitative assessment of mandibular asymmetry using cone beam computed tomography image volumes, Dentomaxillofacial Radiology 40: ((2011) ), 351–357. |
[13] | Cevidanes L.H. , Alhadidi A. , Paniagua B. et al., Three-dimensional quantification of mandibular asymmetry through cone-beam computerized tomography, Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 111: ((2011) ), 757–770. |
[14] | Kim S.-H. , Choi Y.-S. , Hwang E.-H. , Chung K.-R. , Kook Y.-A. and Nelson G. , Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography, American Journal of Orthodontics and Dentofacial Orthopedics 131: ((2007) ), S82–S89. |
[15] | Kim G.-T. , Kim S.-H. , Choi Y.-S. , et al. Cone-beam computed tomography evaluation of orthodontic miniplate anchoring screws in the posterior maxilla, American Journal of Orthodontics and Dentofacial Orthopedics 136: ((2009) ), 628. e621–628. e610. |
[16] | Adibi S. , Zhang W. , Servos T. and O’Neill P.N. , Cone beam computed tomography in dentistry: What dental educators and learners should know, Journal of Dental Education 76: ((2012) ), 1437–1442. |
[17] | Basili C. , Costa H. , Sasaguri K. , Akimoto S. , Slavicek R. and Sato S. , Comparison of the position of the mandibular fossa using 3D CBCT in different skeletal frames in human caucasic skulls, International Journal of Stomatology & Occlusion Medicine 2: ((2009) ), 179–190. |
[18] | Spin-Neto R. , Gotfredsen E. and Wenzel A. , Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: A systematic review, Journal of Digital Imaging 26: ((2013) ), 813–820. |
[19] | Horner K. , O’Malley L. , Taylor K. and Glenny A. , Guidelines for clinical use of CBCT: A review, Dentomaxillofacial Radiology 44: ((2014) ), 20140225. |
[20] | Sekine H. , Miyazaki H. , Takanashi T. et al., Dental implant treatment after improvement of oral environment by orthodontic therapy, The Bulletin of Tokyo Dental College 53: ((2012) ), 109–117. |
[21] | Fuhrmann R. , Three-dimensional interpretation of periodontal lesions and remodeling during orthodontic treatment. Part III, Journal of Orofacial Orthopedics=Fortschritte der Kieferorthopadie: Organ/Official Journal Deutsche Gesellschaft fur Kieferorthopadie 57: ((1996) ), 224–237. |
[22] | Kim Y.I. , Kim M.J. , Choi J.I. et al., A multidisciplinary approach for the management of pathologic tooth migration in a patient with moderately advanced periodontal disease[J], International Journal of Periodontics & Restorative Dentistry 32: ((2012) ), 225–230. |
[23] | Suomalainen A. , Esmaeili E.P. and Robinson S. , Dentomaxillofacial imaging with panoramic views and cone beam CT, Insights into Imaging 6: ((2015) ), 1–16. |
[24] | Chien P. , Parks E. , Eraso F. , Hartsfield J. , Roberts W. and Ofner S. , Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional cone beam computed tomography in vivo, Dentomaxillofacial Radiology 38: ((2009) ), 262–273. |
[25] | Kalender A. , öztan M.D. , Basmaci F. et al., CBCT evaluation of multiple idiopathic internal resorptions in permanent molars: Case report, BMC Oral Health 14: ((2014) ), 1–6. |
[26] | Rugani P. , Kirnbauer B. , Arnetzl G. and Jakse N. , Cone beam computerized tomography: Basics for digital planning in oral surgery and implantology, International Journal of Computerized Dentistry 12: ((2008) ), 131–145. |
Figures and Tables
Fig.1
Comparision of intraoral potographs of pre- and post-treatment. A. Intraoral photographs of pre-treatment; B. Intraoral photographs of post-treatment.

Fig.2
Panoramic radiograph of pre- and post-treatment. A. Panoramic radiograph of pre-treatment; B. Panoramic radiograph of post-treatment. The images showed the relationship between the absorption lines of alveolar bone and the anterior teeth of the uper and lower jaw. The height of alveolar bone in the anterior region was significantly increased.
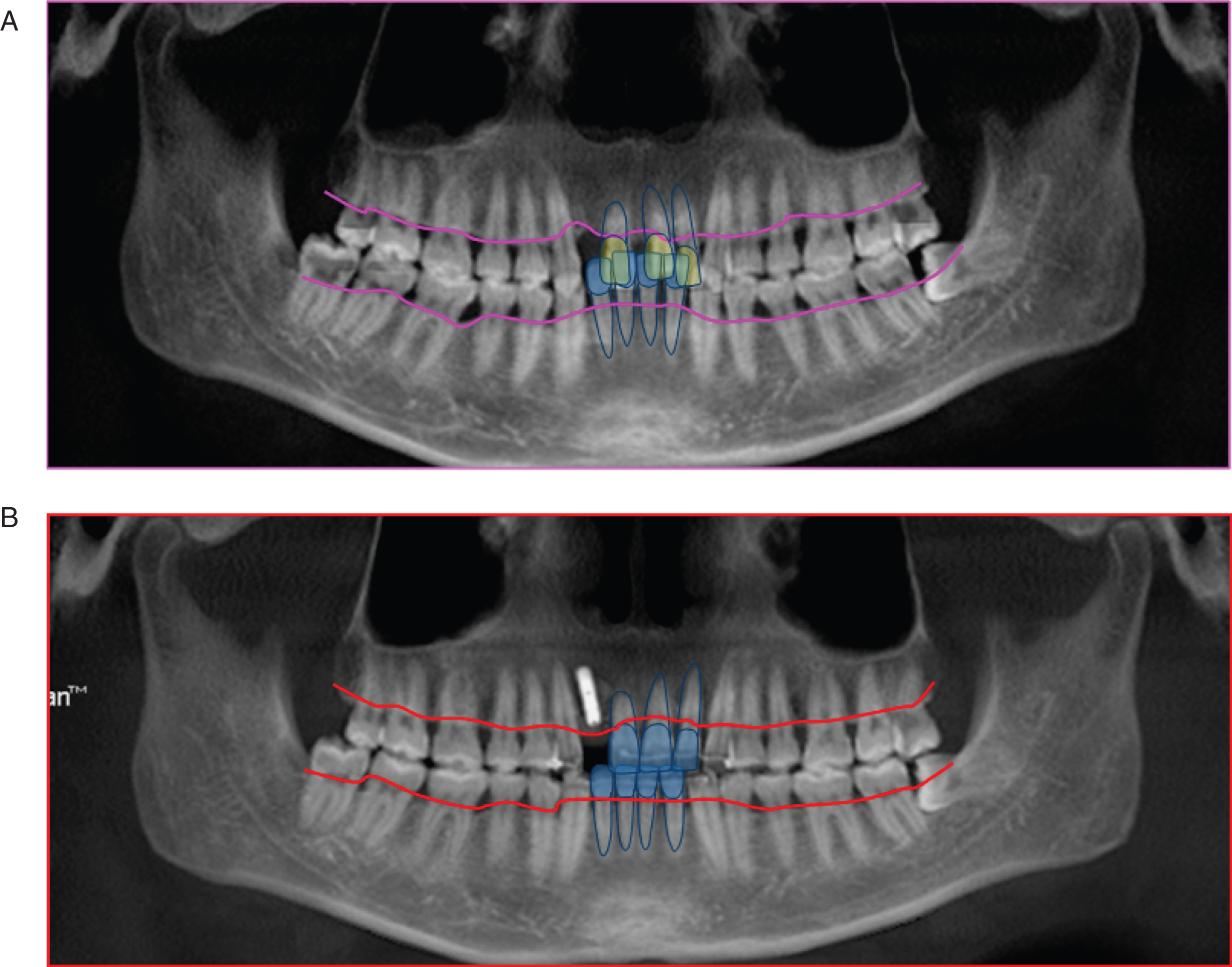
Fig.3
Changes of the anterior region of the maxillary and mandibular teeth. A,B,C,D: static CBCT images of the maxillary right central incisor, maxillary left central incisor, mandibular right central incisor, mandibular left central incisor before treatment; E,F,G,H: static CBCT images of the maxillary right central incisor, maxillary left central incisor, mandibular right central incisor, mandibular left central incisor after treatment; These images showed that no further root absorption was seen in the maxillary right central incisor when the treatment was finished, and the lingual alveolar bone height and thickness was obviously increased in maxillary left central incisor, mandibular right central incisor and mandibular left central incisor.
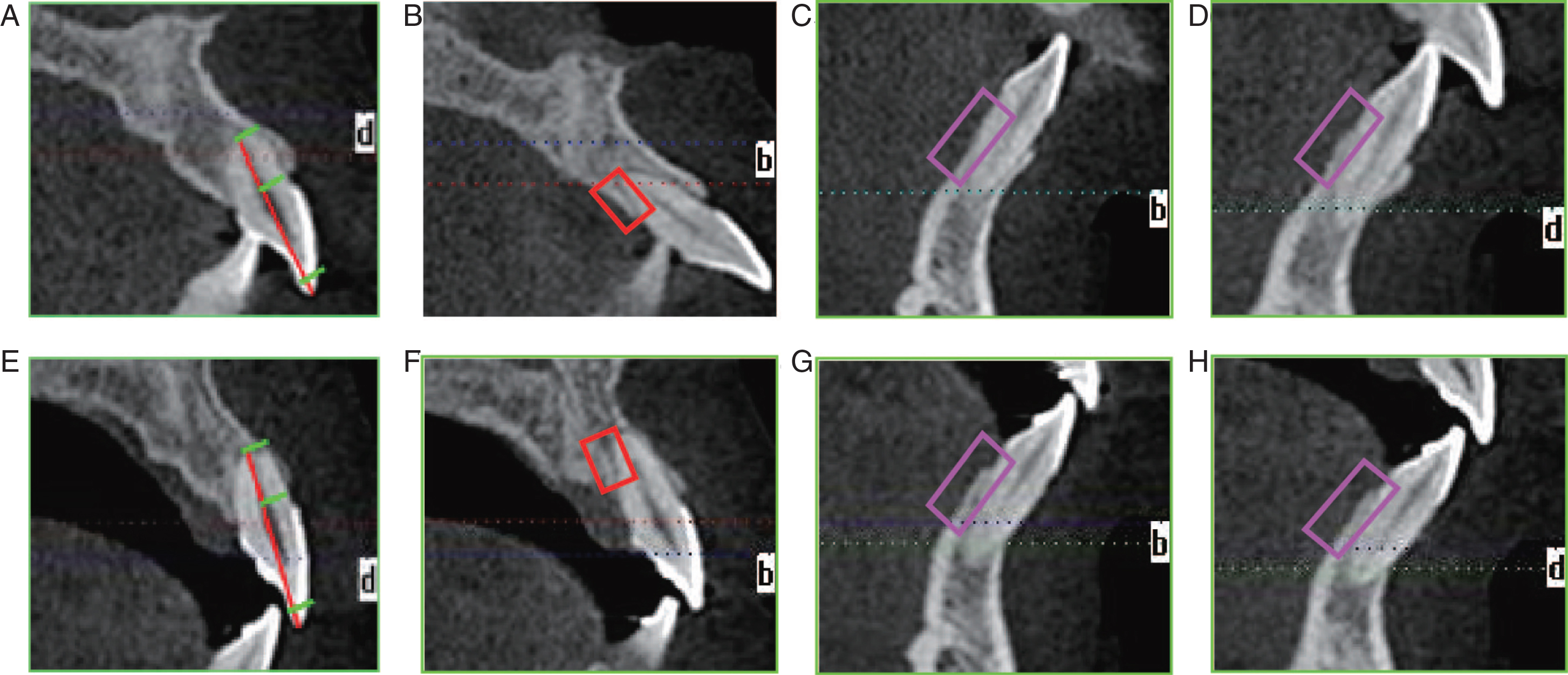
Fig.4
3D rotated images of pre- and post-treatment. A. 3D rotated images of pre-treatment; B. 3D rotated images of post-treatment.
Table 1
Comparison of the advantages and disadvantages of traditional 2D radiographic, traditional CT technology and CBCT
| Radiological technology | Advantages | Disadvantages |
| Traditional 2D radiographs | Could provide 2-dimensional information of the craniofacial region. | Magnification; |
| Geometric distortion; | ||
| Superimposition of structures; Projective displacements. | ||
| Traditional CT technology | Could provide 3-dimensional information of the craniofacial region. | High radiation dose; |
| High cost; | ||
| Long scanning time; | ||
| Certain degree of deformation and artifacts from metal. | ||
| CBCT | Could evaluate the hard and soft tissues of the maxillofacial region in 3 dimensions; | Higher price than traditional 2D radiographs; |
| Could provide spatial details and overall information; | Higher radiation dose than traditional 2D radiographs. | |
| Lower radiation dose than traditional CT; | ||
| Lower cost than traditional CT | ||
| Convenience; | ||
| Accuracy in all three dimension of the alveolar bone; | ||
| Images can be rotated. |



