Association of COVID-19 with New-Onset Alzheimer’s Disease
Abstract
An infectious etiology of Alzheimer’s disease has been postulated for decades. It remains unknown whether SARS-CoV-2 viral infection is associated with increased risk for Alzheimer’s disease. In this retrospective cohort study of 6,245,282 older adults (age ≥65 years) who had medical encounters between 2/2020–5/2021, we show that people with COVID-19 were at significantly increased risk for new diagnosis of Alzheimer’s disease within 360 days after the initial COVID-19 diagnosis (hazard ratio or HR:1.69, 95% CI: 1.53–1.72), especially in people age ≥85 years and in women. Our findings call for research to understand the underlying mechanisms and for continuous surveillance of long-term impacts of COVID-19 on Alzheimer’s disease.
INTRODUCTION
An infectious etiology of Alzheimer’s disease has been postulated for decades and despite supportive evidence, it is still controversial [1]. The increased risk for COVID-19 in people with Alzheimer’s disease [2] and recent recognition of long lasting neurological sequela of SARS-CoV2 infection [3] in part reflecting inflammatory processes, which are central to Alzheimer’s disease neuropathology [4], suggest bidirectional relationships. However, whether COVID-19 might trigger new-onset Alzheimer’s disease or accelerate its emergence is unclear.
METHODS
We used the TriNetX Analytics Platform to access de-identified electronic health records of over 95 million patients of both inpatient and outpatient visits from 68 health care organizations, representing 28% of the US population from 50 states covering diverse geographic, age, race/ethnic, income, and insurance groups [5]. Information on race and ethnicity is provided in Table 1 and the Supplementary Material. TriNetX built-in analytic functions allow for patient-level analyses, while only reporting population level data. The MetroHealth System Cleveland Institutional Review Board determined research using TriNetX is not Human Subject Research and therefore exempt from Institutional Review Board review. We have used TriNetX Analytics network platform in COVID-19 research [6–12], including our recent study showing that fully vaccinated patients with Alzheimer’s disease were at increased risk for breakthrough SARS-CoV-2 infections [9].
Table 1
Characteristics of older adults (age ≥65 y) with versus without COVID-19 before and after propensity-score matching
| Before matching | After matching | |||||
| COVID-19 Cohort | Non-COVID-19 Cohort | SMD | COVID-19 Cohort | Non-COVID-19 Cohort | SMD | |
| Total number | 410,748 | 5,834,534 | 410,478 | 410,478 | ||
| Age (y, mean±SD) | 73.7±7.75 | 73.0±7.34 | 0.10* | 73.7±7.75 | 73.7±7.75 | <0.001 |
| Sex (%) | ||||||
| Female | 53.6 | 55.6 | 0.04 | 53.6 | 53.6 | <0.001 |
| Male | 46.6 | 44.4 | 0.04 | 46.6 | 46.6 | <0.001 |
| Ethnicity (%) | ||||||
| Hispanic | 6.7 | 3.5 | 0.15* | 6.7 | 6.7 | <0.001 |
| Not Hispanic | 68.9 | 63.5 | 0.11* | 68.9 | 68.9 | <0.001 |
| Unknown | 24.4 | 33.0 | 0.19* | 24.4 | 24.4 | <0.001 |
| Race (%) | ||||||
| Asian | 1.6 | 1.7 | 0.002 | 1.6 | 1.6 | 0.001 |
| Black | 10.0 | 7.8 | 0.08 | 10.0 | 10.0 | <0.001 |
| White | 75.3 | 74.1 | 0.03 | 75.3 | 75.4 | <0.001 |
| Unknown | 12.5 | 16.0 | 0.10 | 12.5 | 12.5 | <0.001 |
| Adverse socioeconomic and | 13.2 | 2.9 | 0.39* | 13.2 | 13.2 | <0.001 |
| psychosocial circumstances (%) | ||||||
| Comorbidities | ||||||
| Hypertension | 59.4 | 44.5 | 0.30* | 59.4 | 59.4 | <0.001 |
| Overweight and obesity | 23.0 | 14.4 | 0.22* | 23.0 | 23.1 | <0.001 |
| Type 2 diabetes | 30.4 | 17.9 | 0.29* | 30.4 | 30.4 | <0.001 |
| Depression | 22.1 | 11.5 | 0.29* | 22.1 | 22.2 | <0.001 |
| Hearing loss | 5.9 | 4.9 | 0.04 | 5.9 | 5.8 | 0.002 |
| Traumatic brain injury | 3.3 | 1.5 | 0.12* | 3.3 | 3.1 | 0.007 |
| Tobacco smoking | 10.6 | 7.5 | 0.11* | 10.6 | 10.6 | <0.001 |
| Heavy alcohol drinking | 3.8 | 2.2 | 0.10* | 3.8 | 3.8 | 0.003 |
COVID-19 cohort— contracted COVID-19 between 2/2020–5/2021. Non-COVID-19 cohort— had no documented COVID-19 but had medical encounters with healthcare organizations between 2/2020–5/2021. Self-identified race and ethnicity as recorded in the TriNetX electronic health records database were included because they have been associated with both infection risk and severe outcomes of COVID-19. SMD, standardized mean differences. *SMD greater than 0.1, a threshold being recommended for declaring imbalance.
The study population comprised 6,245,282 older adults (age ≥65 years) who had medical encounters with healthcare organizations between 2/2/2020–5/30/2021 and had no prior diagnosis of Alzheimer’s disease. The population was divided into two cohorts: 1) COVID-19 cohort (n = 410,748)— contracted COVID-19 between 2/2/2020–5/30/2021; 2) non-COVID-19 cohort (n = 5,834,534)— had no documented COVID-19 but had medical encounters with healthcare organizations between 2/2/2020–5/30/2021. The status of Alzheimer’s disease and COVID-19 were based on the International Classification of Diseases (ICD-10) diagnosis codes and laboratory tests (details in the Supplementary Material).
We examined risks for new diagnosis of Alzheimer’s disease in COVID-19 and non-COVID-19 cohorts in all older adults, three age groups (65–74, 75–84, ≥85), and three racial/ethnic groups (Black, White, and Hispanic). Cohorts were propensity-score matched (1:1 using a nearest neighbor greedy matching) for demographics, adverse socioeconomical determinants of health including problems with education, occupational exposure, physical, social and psychosocial environment, and known risk factors for Alzheimer’s disease [13] (details in the Supplementary Material). Kaplan-Meier analysis was used to estimate the probability of new diagnosis of Alzheimer’s disease within 360 days after the COVID-19 diagnosis. Cox’s proportional hazards model was used to compare matched cohorts using hazard ratios and 95% confidence intervals. All statistical tests were conducted within the TriNetX Advanced Analytics Platform at significance set at p < 0.05 (2-sided). The TriNetX platform calculates HRs and associated CIs using R’s Survival package, version 3.2-3. Details of the TriNetX database, study population, and statistical methods are in the Supplementary Material.
RESULTS
Patient characteristics
The study population comprised 6,245,282 older adults (age ≥65 years) including 410,748 in the COVID-19 cohort and 5,834,534 in the non-COVID-19 cohort. The COVID-19 cohort did not differ in age nor gender from the non-COVID-19 cohort, but comprised more Hispanic and Black people and had higher prevalence of adverse socioeconomic determinants of health and comorbidities. After matching, the COVID-19 and non-COVID-19 cohorts were balanced (Table 1).
Increased risk of new diagnosis of Alzheimer’s disease among patients with COVID-19 compared to propensity-score matched patients without COVID-19
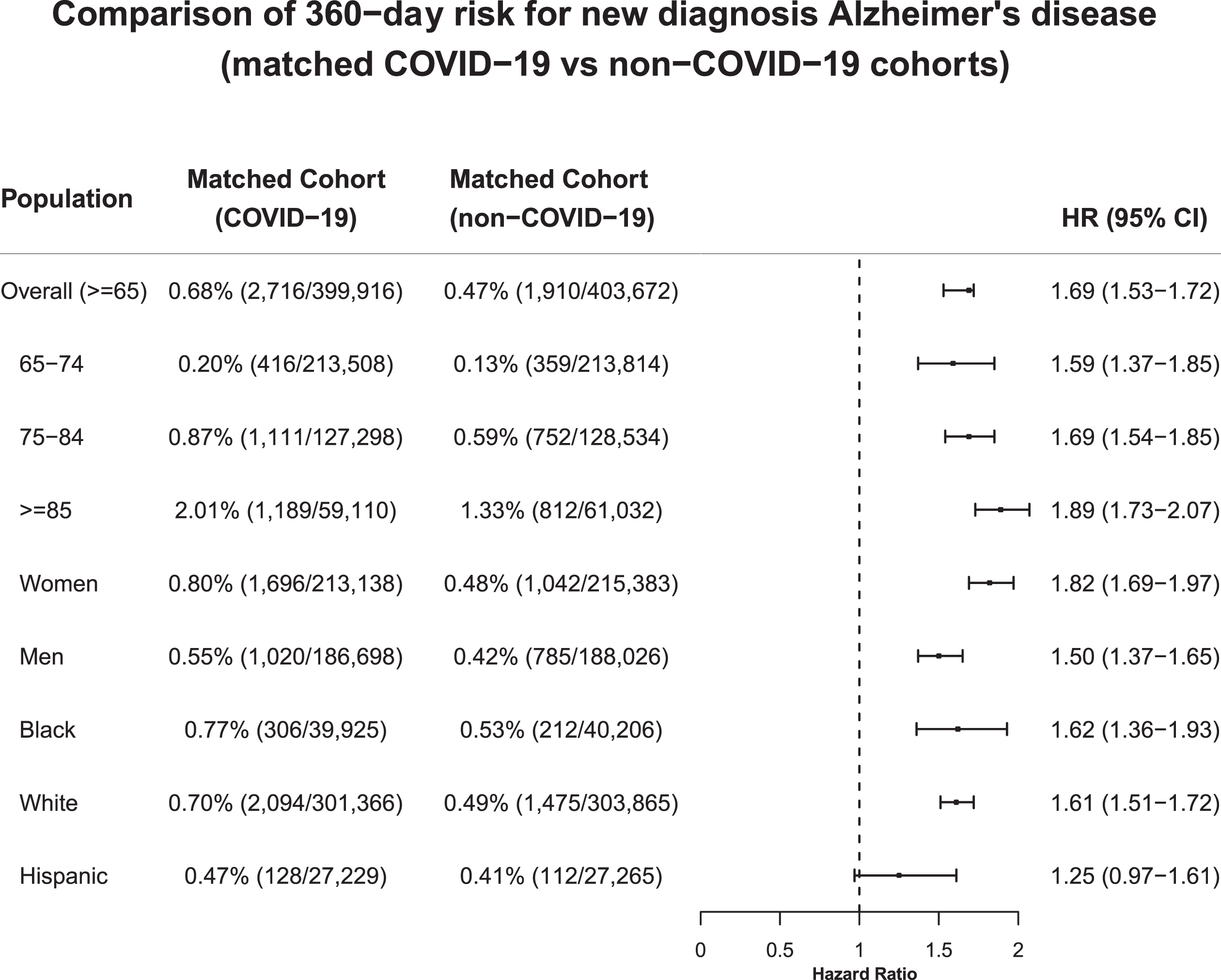
Before propensity-score matching the overall risk for new diagnosis of Alzheimer’s disease in the COVID-19 cohort was 0.68%, compared to 0.35% in the non-COVID-19 cohort. After propensity-score matching, COVID-19 cohort had increased risk for new diagnosis of Alzheimer’s disease compared to matched non-COVID-19 cohort (HR: 1.69, 95% CI: 1.53–1.72). Increased risk was observed in populations stratified by age groups (65–74, 75–84, ≥85), gender (women, men), and race or ethnicity (Black, White, Hispanic), with highest risk in people age ≥85 years (HR: 1.89, 95% CI: 1.73–2.07) and in women (HR: 1.82, 95% CI: 1.69–1.97) (Fig. 1).
Fig. 1
Comparison of 180-day risk for new diagnosis of Alzheimer’s disease between propensity-score matched COVID-19 and non-COVID-19 cohorts. COVID-19 cohort— older adults (age ≥65) who contracted COVID-19 between 2/2020–5/2021. Non-COVID-19 cohort— older adults (age ≥65) who had no documented COVID-19 in their EHRs but had medical encounters with healthcare organizations between 2/2020–5/2021. Cohorts were propensity-score matched for demographics (age, gender, race/ethnicity), socioeconomic factors and Alzheimer’s disease-related comorbidities and behavioral factors as per Table 1.
DISCUSSION
Older adults with COVID-19 were at significantly increased risk for new diagnosis of Alzheimer’s disease with highest risk in people age ≥85 and in women. Study limitations include potential biases introduced by the observational and retrospective nature of this study and inaccuracy in Alzheimer’s disease diagnosis, which should not substantially affect the relative risk analyses since all cohorts were drawn from the same dataset. Next steps include validation from other data resources, longer-term follow-up, mechanism understanding and examining other types of dementia
ACKNOWLEDGMENTS
We acknowledge support from National Institute on Aging (grants nos. AG076649, AG057557, AG061388, AG062272), National Institute on Alcohol Abuse and Alcoholism (grant no. R01AA029831), the Clinical and Translational Science Collaborative (CTSC) of Cleveland (grant no. 1UL1TR002548-01), and National Cancer Institute Case Comprehensive Cancer Center (R25CA221718, P30 CA043703, P20 CA2332216)
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/22-0717).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-220717.
REFERENCES
[1] | Itzhaki RF , Golde TE , Heneka MT , Readhead B ((2020) ) Do infectionshave a role in the pathogenesis of Alzheimer disease? Nat RevNeurol 16: , 193–197. |
[2] | Wang Q , Davis PB , Gurney ME , Xu R ((2021) ) COVID-19 and dementia: Analyses of risk, disparity, and outcomes from electronic health records in the US. Alzheimers Dement 17: , 1297–1306. |
[3] | Boldrini M , Canoll PD , Klein RS ((2021) ) How COVID-19 affects the brain. JAMA Psychiatry 78: , 682–683. |
[4] | Frost GR , Jonas LA , Li Y-M ((2019) ) Friend, foe or both? Immune activity in Alzheimer’s disease. Front Aging Neurosci 11: , 337. |
[5] | TriNetX, https://trinetx.com/. Accessed June 2022. |
[6] | Wang L , Wang Q , Davis PB , Volkow ND , Xu R ((2022) ) Increased risk for COVID-19 breakthrough infection in fully vaccinated patients with substance use disorders in the United States between December 2020 and August 2021. World Psychiatry 21: , 124–132. |
[7] | Wang L , Berger NA , Kaelber DC , Davis PB , Volkow ND , Xu R XuR(2022) Incidence rates and clinical outcomes of SARSCoV-2 infection with the omicron and delta variants in children younger than 5 years in the US. JAMA Pediatr. doi: 10.1001/jamapediatrics.2022.0945. |
[8] | Wang L , Davis PB , Kaelber DC , Volkow ND , Xu R ((2022) ) Comparison of mRNA-1273 and BNT162b2 vaccines on breakthrough SARS-CoV-2 infections, hospitalizations, and death during the delta-predominant period. JAMA 327: , 678–680. |
[9] | Wang L , Davis PB , Kaelber DC , Xu R (2022) COVID-19 breakthrough infections and hospitalizations among vaccinated patients with dementia in the United States between December 2020 and August 2021. Alzheimers Dement. doi: 10.1002/alz.12669. |
[10] | Wang W , Kaelber DC , Xu R , Berger NA (2022) Breakthrough SARS-CoV-2 infections, hospitalizations, and mortality in vaccinated patients with cancer in the US between December 2020 andNovember 2021. JAMAOncol. doi: 10.1001/jamaoncol.2022.1096. |
[11] | Wang L , Kaelber DC , Xu R , Berger NA ((2022) ) COVID-19 breakthrough infections, hospitalizations and mortality in fully vaccinated patients with hematologic malignancies: A clarion call for maintaining mitigation and ramping-up research. Blood Rev 54: , 100931. |
[12] | Wang L , Berger NA , Xu R ((2021) ) Risks of SARS-CoV-2 breakthrough infection and hospitalization in fully vaccinated patients with multiple myeloma. JAMA Netw Open 4: , e2137575. |
[13] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C , Costafreda SG , Dias A , Fox N , Gitlin LN , Howard R , Kales HC , Kivimäki M , Larson EB , Ogunniyi A , Orgeta V , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbæk G , Teri L , Mukadam N ((2020) ) Dementiaprevention, intervention, and care: 2020 report of the LancetCommission. Lancet 396: , 413–446. |



