Nutritional Intervention to Prevent Alzheimer’s Disease: Potential Benefits of Xanthophyll Carotenoids and Omega-3 Fatty Acids Combined
Abstract
Background:
A growing body of scientific evidence suggests that enrichment of certain nutritional compounds in the brain may reduce the risk of Alzheimer’s disease (AD).
Objective:
To investigate the impact of supplemental xanthophyll carotenoids plus omega-3 fatty acids on disease progression in patients with AD.
Methods:
Three trial experiments were performed. In Trials 1 and 2 (performed on patients with AD over an 18-month period), 12 patients (AD status at baseline: 4 mild and 8 moderate) were supplemented with a xanthophyll carotenoid only formulation (Formulation 1; lutein:meso-zeaxanthin:zeaxanthin 10:10:2 mg/day) and 13 patients (AD status at baseline: 2 mild, 10 moderate, and 1 severe) were supplemented with a xanthophyll carotenoid and fish oil combination (Formulation 2; lutein:meso-zeaxanthin:zeaxanthin 10:10:2 mg/day plus 1 g/day of fish oil containing 430 mg docohexaenoic acid [DHA] and 90 mg eicopentaenoic acid [EPA]), respectively. In Trial 3, 15 subjects free of AD (the control group) were supplemented for 6 months with Formulation 1. Blood xanthophyll carotenoid response was measured in all trials by HPLC. Omega-3 fatty acids were profiled by direct infusion mass spectrometry.
Results:
Xanthophyll carotenoid concentration increases were significantly greater for Formulation 2 compared to Formulation 1 (p < 0.05), and progression of AD was less for this group (p = 0.003), with carers reporting functional benefits in memory, sight, and mood.
Conclusion:
This preliminary report suggests positive outcomes for patients with AD who consumed a combination of xanthophyll carotenoids plus fish oil, but further study is required to confirm this important observation.
INTRODUCTION
Dementia is a neuropsychiatric syndrome characterized by a combination of cognitive decline, progressive behavioral and psychological symptoms (BPSD) and functional disability [1]. Alzheimer’s disease (AD) is the most common type of dementia (accounting for approximately 60–70% of cases), followed by vascular dementia. Dementia represents a major cost burden for healthcare providers. In 2016, the World Alzheimer Report showed that the current annual societal and economic cost of dementia was US$818 billion, and that it is expected to become a trillion-dollar disease this year (2018) [2]. The cost of dementia is the result of direct (e.g., hospital care, community services, nursing homes) [3] and indirect costs (e.g., caregivers contribution) [4].
The exact cause of dementia is unknown, but established risk factors include age, family history of disease, and education [5], and putative risk factors include cigarette smoking, physical inactivity, and social isolation [6]. For AD, the effectiveness of current pharmacological treatments (medications) is limited and varies among individuals. The effect of current medications at best is only palliative, as they cannot halt disease progression. The UK NHS suggests, as preventative, the following: cessation of smoking, limiting alcohol, a healthy well-balanced diet, staying physically and mentally active. Unless new strategies for prevention and management are developed, this syndrome is expected to continue to place growing demands on healthcare and society as a whole.
There is now a growing body of scientific evidence which suggests that enrichment of certain nutritional compounds in the brain may play a role in reducing the risk of AD [7]. Several large prospective observational studies conclude that adherence to a healthy diet, such as the Japanese diet [8] or the Mediterranean diet [9] can reduce risk of AD. Of note, there have been several studies on the Mediterranean diet, characterized by a high intake of vegetables, olive oil, and a moderate intake of fish, dairy products, and wine, which show that adherence to such diets is associated with better cognitive performance [10–14] and a reduced risk of dementia, especially AD [9, 15–18], but no clear evidence of the exact foodstuffs responsible. It is our view that the challenge is therefore to identify the exact nutrients within these diets that are responsible for protecting the brain from degeneration. Achieving this goal would allow for targeted nutritional supplementation for patients with, or at risk of, AD, and thereby reduce the burden of the disease.
To date, the most promising leads have been with omega-3 fatty acids, which include docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). These fatty acids are found in high concentrations in fish oil and in fatty fish such salmon and herring. There is a substantial concentration of DHA in the brain where it forms a structural component within this neural tissue. High consumption of omega-3 fatty acids is associated with better cognitive performance [19] and a reduced risk of dementia [20–24]. However, interventional studies have shown conflicting results, with some demonstrating improvements in cognition [25, 26] and others demonstrating no beneficial effect [27, 28].
Other food items (nutrients) of interest include the xanthophyll carotenoids lutein (L), zeaxanthin (Z), and meso-zeaxanthin (MZ). L and Z are found in certain fruits and vegetables (e.g., spinach, broccoli, peppers, melon) [29]; whereas, MZ has been identified in fish [30] and is also believed to be generated from L at the retina [31]. In the human, these carotenoids are found in high concentrations at the macula (the center part of the retina, where they are referred to as macular pigment [MP]) and L and Z have been identified in the brain [32, 33]. High xanthophyll carotenoid intake has been found to result in a reduced risk of AD [34–36]. Indeed, interventional studies administering L and Z have shown improvement in different domains of cognition in patients free of AD [37–39]. However, a randomized clinical trial performed by our group in patients with AD who were supplemented with xanthophyll carotenoids found no benefit in measures of cognitive function performed in that trial [40].
In summary, there is general agreement that there are nutritional compounds in the brain which play a role in preventing AD [7], but attempts so far to identify these exact nutrients, and use them to prevent AD have been unsuccessful. We propose here that we have identified “a synergistic nutritional strategy” via a unique combination of xanthophyll carotenoids and omega-3 fatty acids to potentially slow the progression rate of AD and aid in the management of this disease. The preliminary trial data are presented below.
MATERIALS AND METHODS
Study sample
This research was conducted at the Nutrition Research Centre Ireland (NRCI; http://www.nrci.ie) in collaboration with University Hospital Waterford (UHW), South East, Republic of Ireland. Patients with AD were recruited (for Trials 1 and 2, see below) from UHW via the Age-Related Care Unit department. Subjects for the control group (Trial 3, see below) were recruited via newspaper and radio advertisements, and by word of mouth in the local community. This study was conducted in accordance with full sensitivity to the ethical requirements of the patients recruited. The study objectives and methodology complied fully with the widely-recognized international text and codes of practice, such as the Declaration of Helsinki and Good Research Practice. A protocol for obtaining informed consent was developed specifically for this trial by the Principal Investigator (JMN) of the NRCI and Consultant Geriatrician (RM) of the UHW to ensure that the protocol was safe and appropriate, and in keeping with the ethical code germane to obtaining consent from vulnerable subjects (which includes patients with AD). The protocol for obtaining informed consent was assessed and approved by the local ethics committee prior to the study commencing [41]. The first ethical approval for the Carotenoids And Retinal Dementia Study (CARDS) was granted by local research ethics committee, Health Services Executive, South Eastern Area on 23 August 2012 and duration extension requests/amendments were granted on 14 January 2013, 30 October 2013, 6 May 2014, and the 27 May 2015.
Study trials
In brief, three trial experiments were performed. Two trials were conducted in patients with AD and one trial in age-matched control subjects (free of AD). In Trial 1, 12 patients with AD (4 mild and 8 moderate) were supplemented with a xanthophyll carotenoid only formulation (Formulation 1) over an 18-month period. For note, these 12 patients were followed from the original CARDS sample of 16 [40], as they were available and agreed to continue for the longitudinal 18-month intervention. The daily formulation in Trial 1 was 10 mg L, 10 mg MZ, and 2 mg of Z. In Trial 2, 13 patients with AD (2 mild, 10 moderate, and 1 severe) were supplemented with a xanthophyll carotenoid and fish oil combination (Formulation 2) over an 18-month period. For note, these 13 patients were followed from an original sample of 21 patients from our work (yet unpublished) designed to investigate the impact of xanthophyll carotenoid plus fish oil on phospholipid profile in patients with AD, as these patients were available and agreed to continue for the longitudinal 18-month intervention. The daily formulation in Trial 2 was 10 mg L, 10 mg MZ, and 2 mg of Z plus 1 gram of fish oil (430 mg DHA and 90 mg EPA). In Trial 3, 15 subjects free of AD (the control group) were supplemented for 6 months only using the same intervention as described above for Trial 1 (i.e., Formulation 1), and data from this trial has already been published [40]. Both study formulations were provided as a softgel capsules.
Xanthophyll carotenoids
Assessment performed at baseline and after 6 months of supplementation. Non-fasting blood samples were collected in 9 ml vacuette tubes containing a ‘Z Serum Sep Clot Activator’, and collection tubes were inverted circa 6 times. The blood samples were allowed to clot at room temperature for approximately 30 min and then centrifuged at 2700 rpm for 10 min in a Gruppe GC 12 centrifuge (Desaga Sarstedt) to separate the serum from the whole blood. The resulting serum samples were stored at circa –80°C until the time of batch analysis using high performance liquid chromatography (HPLC). First, the serum samples were analyzed for L and total Z (co-eluted Z and MZ) using a reversed-phase HPLC method (Assay 1) [41]. The mixed Z fraction was automatically collected from Assay 1 using an Agilent 1260 fraction collector. The eluent was dried under a solvent concentrator (MiVac, GeneVac, Mason Technologies, Dublin, Ireland) and analyzed on Assay 2 for quantification of Z and MZ (Assay 2) [42].
Omega-3 fatty acid
Assessment performed at baseline and after 6 months of supplementation. For Trial 2, non-fasting venous blood samples were collected into 6 ml lithium heparin tubes for lipid analysis. Collection tubes were inverted 8–10 times to ensure thorough mixing and centrifuged at 4°C at 3000 rpm for 20 min to separate red blood cells and plasma from whole blood. The time of blood collection and time of separation did not exceed 2 h. Plasma was aliquoted to microtubes and stored at –80°C until further analysis. Lipids were profiled at the Medical Research Council Human Nutrition Research, Cambridge, UK by direct infusion mass spectrometry as described previously [43].
Macular pigment: Central nervous system xanthophyll carotenoid status
MP was measured using the Heidelberg Spectralis® HRA+OCT Multicolor (Heidelberg Engineering GmbH, Heidelberg, Germany). This new technology utilizes confocal scanning laser ophthalmoscopy (cSLO) imaging with diode lasers and uses dual-wavelength autofluorescence (AF) for measuring MP. Dual-wavelength AF in this device uses two excitation wavelengths, one that is well-absorbed by MP (488 nm, blue), and one that is not well absorbed by the pigment (518 nm, green). Of note, the AF method utilized in this study has previously been tested and validated [44]. The Heidelberg Spectralis® provides an image of MP across its spatial profile, but here we report just central MP (at 0.23° eccentricity) and MP volume (calculated as MP average times the area under the curve out to 7° eccentricity).
Dietary intake of xanthophyll carotenoids
A subject’s weekly intake of carotenoid-rich foods (eggs, broccoli, corn, dark leafy vegetables) was inputted into the “L/Z screener” to provide a carotenoid-based diet score. The L and Z values used in the screener were those reported by Perry et al. [43]. This method of assessing and controlling for dietary intake of xanthophyll carotenoids has been used with success elsewhere [12]. Values are weighted for frequency of intake of the food and for bioavailability of L and Z within these foods. A ranking score reflecting the relative intakes (representing arbitrary units) was generated and used in analysis. For the AD subjects, dietary habits were confirmed by a family member or carer. The range of scores on the L/Z screener is 0 to 75. After adding foods with known concentrations of the L and Z into the screener, the following estimates can be made: a low dietary xanthophyll carotenoid intake score ranges from 0–15 (≤2 mg/day); a medium dietary xanthophyll carotenoid score ranges from 16–30 (3–13 mg/day); and a high dietary xanthophyll carotenoid intake score ranges from 31–75 (>13 mg/day).
Clinical/functional assessment
A clinical and functional assessment of each patient was performed at baseline and after 18-months of supplementation. Clinical assessment was performed by a qualified AD nurse (MB) under the supervision of a medical consultant (RM). Also, the patient carer (i.e., the primary person responsible for caring for the patient) was interviewed after 18 months of the patient taking the supplement. AD status at baseline was confirmed by the medical consultant. The Mini-Mental State Examination (MMSE) was used to guide the diagnosis of AD during patient recruitment (baseline). With MMSE, AD status is defined as follows: 21–25 = Mild AD; 11–20 = Moderate AD; 0–10 = Severe AD. Of note, MMSE data was not obtained at 18 months as this is not part of routine medical assessment at UHW. For our report, AD status was coded as follows: Mild = 0; Moderate = 1; Advanced = 2. AD status was provided by the research nurse (MB) under the guidance and supervision of the medical consultant and guided by all information available to the research team (i.e., MMSE; clinical story; mood; function). Health status and assessment of each patient was performed after 18 months, where possible. To achieve this, the research nurse interviewed the carer of the patient to assess health status and patient function. Notes were recorded from each assessment. Importantly, the research nurse confirmed that the carer was the same person at baseline and 18-month follow up.
Statistical analysis
The statistical package IBM SPSS version 22 was used, and the 5% significance level applied, for all analyses. SigmaPlot version 8.0 was used to generate line graphics for presentation. Results were expressed as means±standard deviations in tables and means±standard errors for graphics. Between-group differences were analyzed using Independent Samples t-tests, One-way analysis of variance (ANOVA) or chi-square tests as appropriate. Repeated measures analyses of variance (rANOVA) was used to assess Time and/or Time-Group interaction effects between the treatment intervention groups for serum concentrations of L, Z and MZ. Time effects examine whether or not a response variable is different at the various time points of interest. Time-Group effects examine whether or not the time effect differs between the treatment intervention groups, therefore testing the impact of the intervention.
RESULTS
Baseline
Table 1 below presents baseline data for AD patients and control subjects enrolled into the three Trials. As seen in this table, the patients with AD in Trial 1 and Trial 2 were comparable in age, sex, BMI, dietary L/Z intake, serum Z concentrations and AD category. Patients in Trial 2 had significantly lower blood L concentrations than patients in Trial 1 (p = 0.031). Other observations of note at baseline were the positive and statistically significant relationships between dietary L and Z intake and serum concentrations of L and Z (r = 0.601, p = 0.000 and r = 0.330, p = 0.043, respectively).
Table 1
Demographic, AD status and biochemical health variables for patients recruited into the Trials at baseline
| Demographic and health variables | Trial 1 (n = 12): AD | Trial 2 (n = 13): AD | Trial 3 (n = 15): Controls | Comparison AD groups | Comparison all groups |
| Age (years) | 78.5±8.754 | 78.77±7.65 | 77±7.4 | p = 0.935 | p = 0.444 |
| Sex (% females) | 6 (50%) | 8 (71%) | 6 (40%) | p = 0.561 | p = 0.524 |
| Dietary L/Z | 14.9±0.8.78 | 13.69±10.1 | 21.92±14.72 | p = 0.751 | p = 0.156 |
| Serum L (μmol/L) | 0.261±0.142 | 0.154±0.084 | 0.275±0.175 | p = 0.031 | p = 0.068 |
| Serum Z (μmol/L) | 0.048±0.035 | 0.062±0.031 | 0.066±0.035 | p = 0.297 | p = 0.409 |
| BMI | 24.6±3 | 24.4±3 | 27.17±3 | p = 0.863 | p = 0.078 |
| MMSE category | 19±2.89 | 16±2.873 | 29±1.311 | p = 0.140 | p = 0.000 |
| Mild AD | 4 (33%) | 2 (15%) | na | p = 0.105 | – |
| Moderate AD | 8 (67%) | 10 (77%) | na | p = 0.105 | – |
| Severe AD | 0 (0%) | 1 (8%) | na | p = 0.105 | – |
| MP 0.23 | 0.41±0.24 | – | 0.55±0.17 | – | p = 0.097 |
| MP Volume | 4114±2308 | – | 6092±2421 | – | p = 0.019 |
| DHA | – | 0.160±0.118 | – | – | – |
| EPA | – | 0.153±0.144 | – | – | – |
AD, Alzheimer’s disease; Trial 1, patients with AD supplemented with Formulation 1; Formulation 1, 10 mg lutein, 10 mg meso-zeaxanthin, and 2 mg of zeaxanthin (carotenoid only); Trial 2, patients with AD supplemented with Formulation 2; Formulation 2, 10 mg lutein, 10 mg meso-zeaxanthin, and 2 mg of zeaxanthin plus 1 gram of fish oil (430 mg docohexaenoic acid [DHA] and 90 mg eicopentaenoic acid [EPA]) (carotenoid plus fish oil); Trial 3, aged-matched control subjects supplemented with Formulation 1; Dietary L/Z, a dietary score for lutein and zeaxanthin intake (see methods); Serum L and Z, serum concentration of lutein and zeaxanthin measured in μmol/L; BMI, body mass index expressed in units of kg/m2; MMSE, Mini-Mental State Examination; MP 0.23, macular pigment at center (0.23 degrees of retinal eccentricity); MP volume, macular pigment average times the area under the curve; DHA, LPC 22:6 phospholipid; EPA, LPC 20:5 phospholipid.
Biochemical response: Xanthophyll carotenoids and omega-3 fatty acids
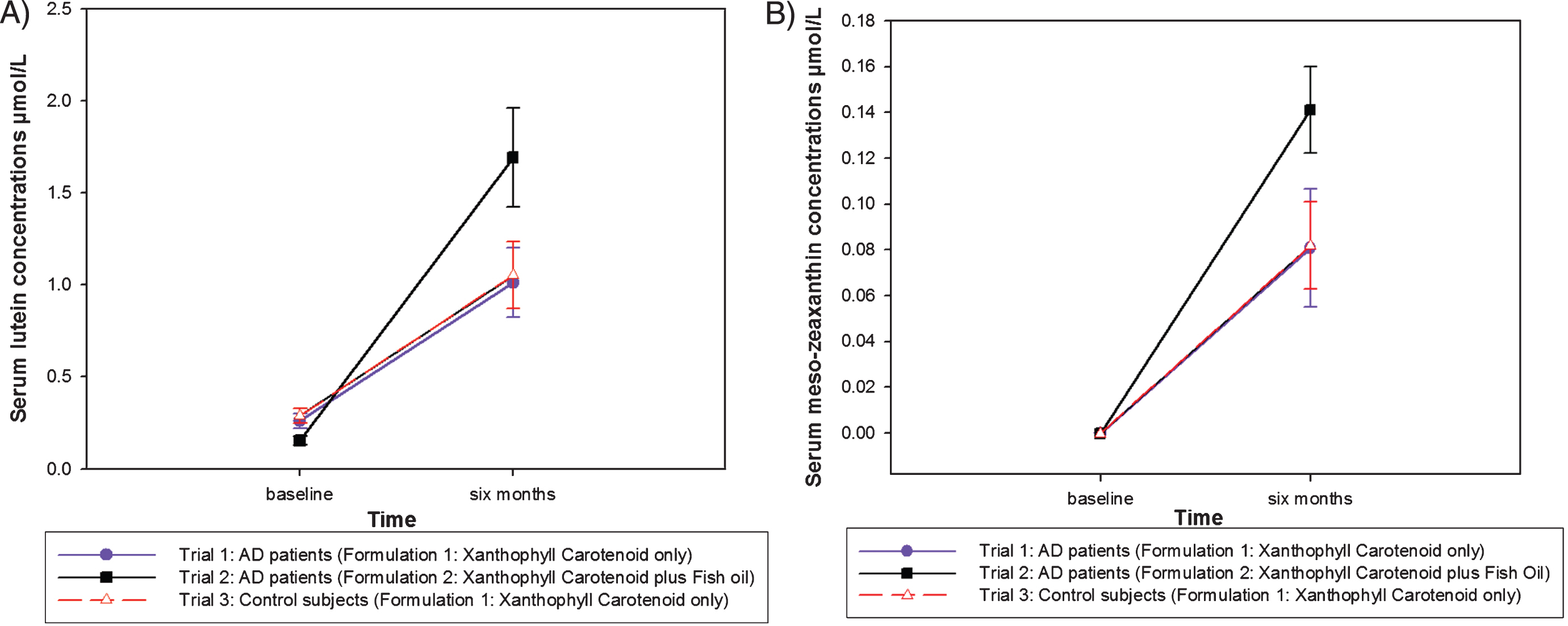
The increase observed in L and MZ concentrations was significantly greater in the AD patients that were supplemented with the combination of xanthophyll carotenoids plus omega-3 fatty acids (Formulation 2), when compared to the AD patients that were supplemented with the xanthophyll carotenoids only formulation (Formulation 1) and when compared to the control group that were supplemented with the xanthophyll carotenoid only formulation (Formulation 1) (serum L: p = 0.002, Fig. 1A; serum MZ: p = 0.006, Fig. 1B).
Fig.1
A. Serum lutein response after six months for each trial group. B. Serum meso-zeaxanthin response after six months for each trial group.
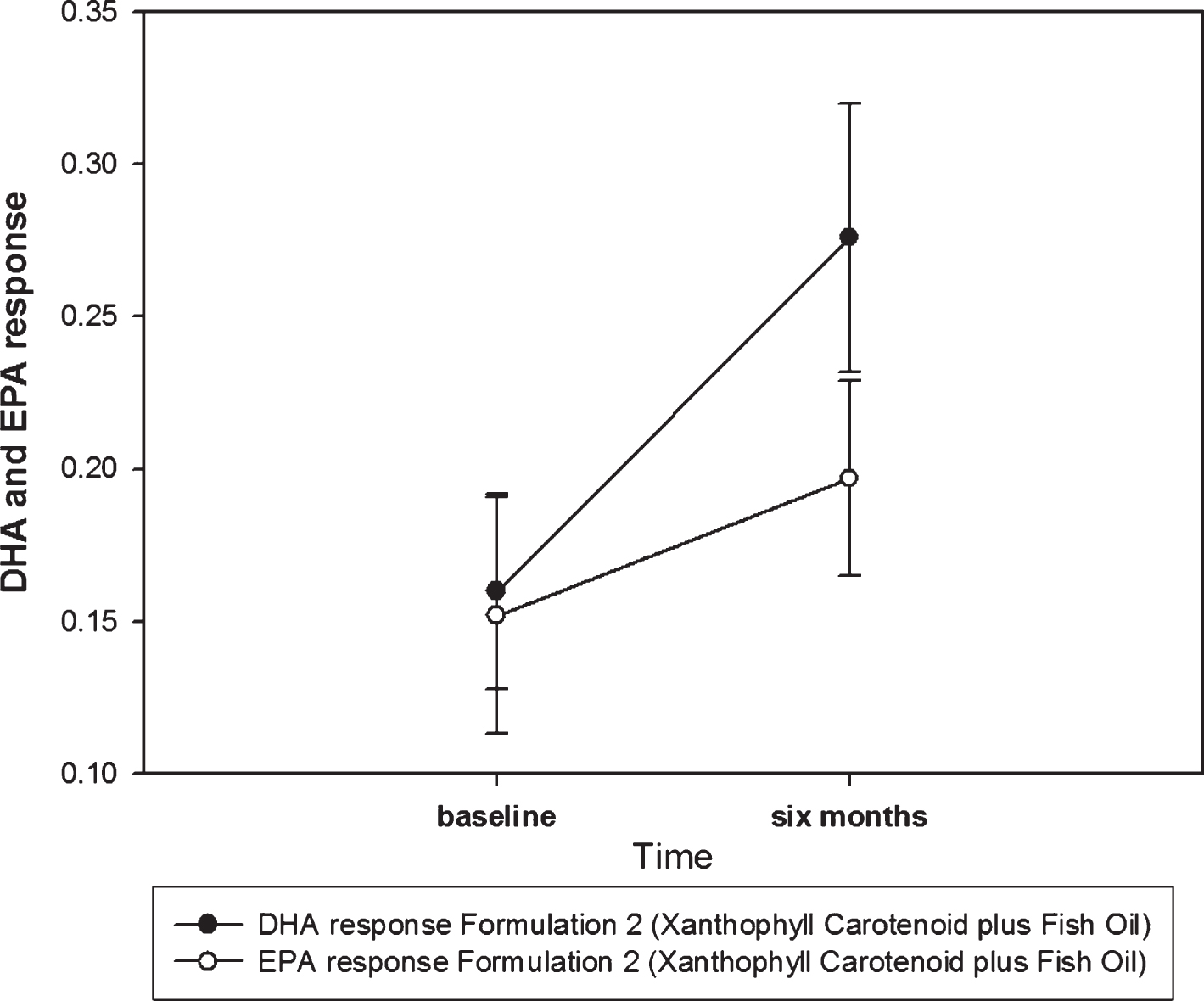
Also, for Trial 2, DHA and EPA concentrations increased in the blood of the AD patients (of note, DHA and EPA measurements were only performed in this trial because the other trials did not have DHA or EPA in the supplement formulation). The increase observed in DHA, the main component of the fish oil used in Formulation 2, was statistically significant (p = 0.041, see Fig. 2).
Fig.2
DHA and EPA response for Trial 2. The data presented here is LPC 22:6 (phospholipid containing DHA) = phospholipid containing DHA relative to the total lipid signal in blood and LPC 20:5 (phospholipid containing EPA) = phospholipid containing EPA relative to the total lipid signal in blood. These are excellent biomarkers of DHA and EPA.
Clinical/functional response in patients with Alzheimer’s disease
Figures 3A and 3B present the AD status for Trial 1 at baseline and 18-months, respectively. Figures 4A and 4B present the AD status for Trial 2 at baseline and 18-months, respectively. Of note, data at 18-months represents medical observations and patient health status (see Table 2). As seen from the pie charts (Fig. 3A, B) and Table 2, progression of AD was evident in this group (data from Trial 1, xanthophyll carotenoid only intervention) over the 18-month period, with 42% of patient’s health status dropping to the point that they could not continue in the trial. Reasons for dropout included: patient moved into a nursing home due to AD progressing and unable to take the supplement; patient became too unwell to continue; cognitive decline too severe; no longer able to follow instructions.
Fig.3
A. Trial 1 - Baseline AD status. B. Trial 1 – 18-month findings.
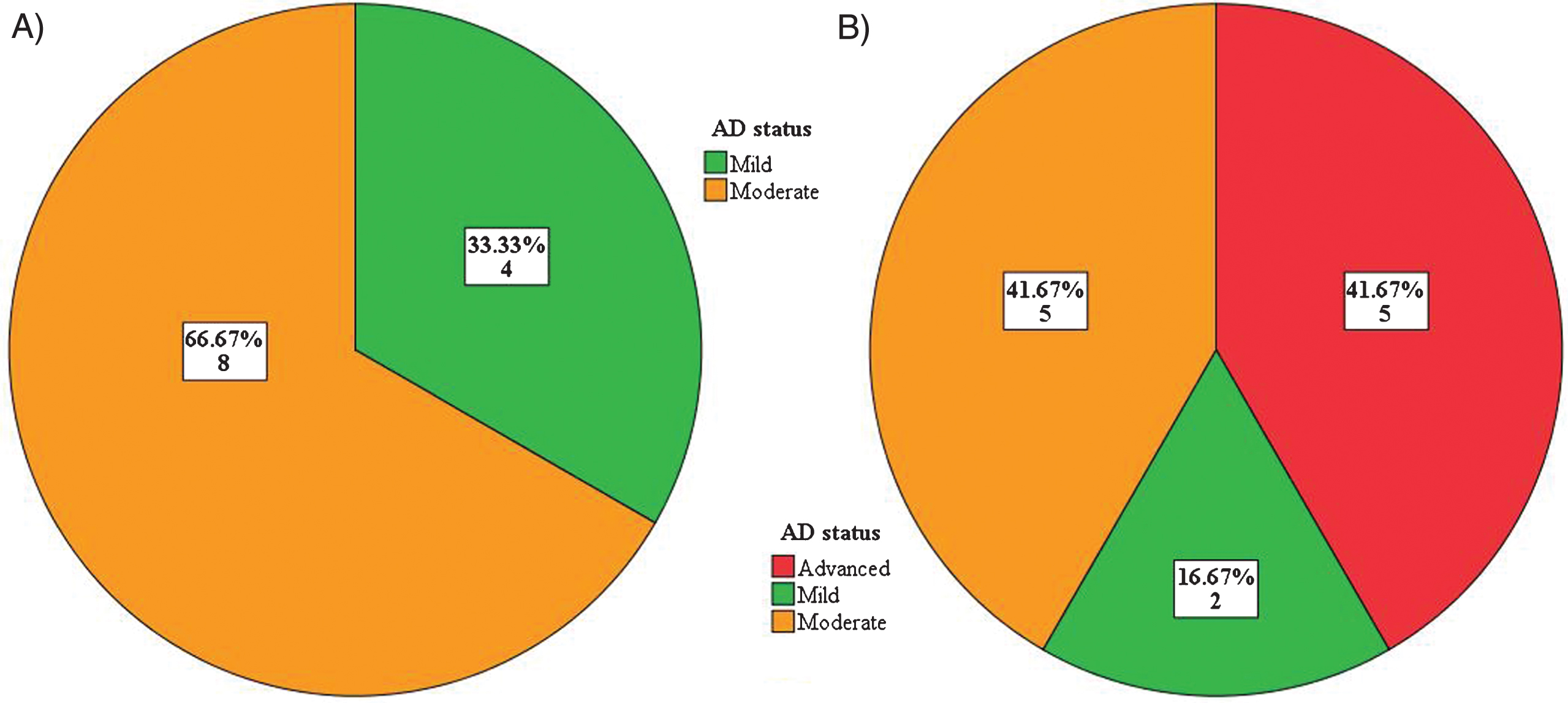
Fig.4
A. Trial 2 – Baseline AD status. B. Trial 2 – 18-month findings.
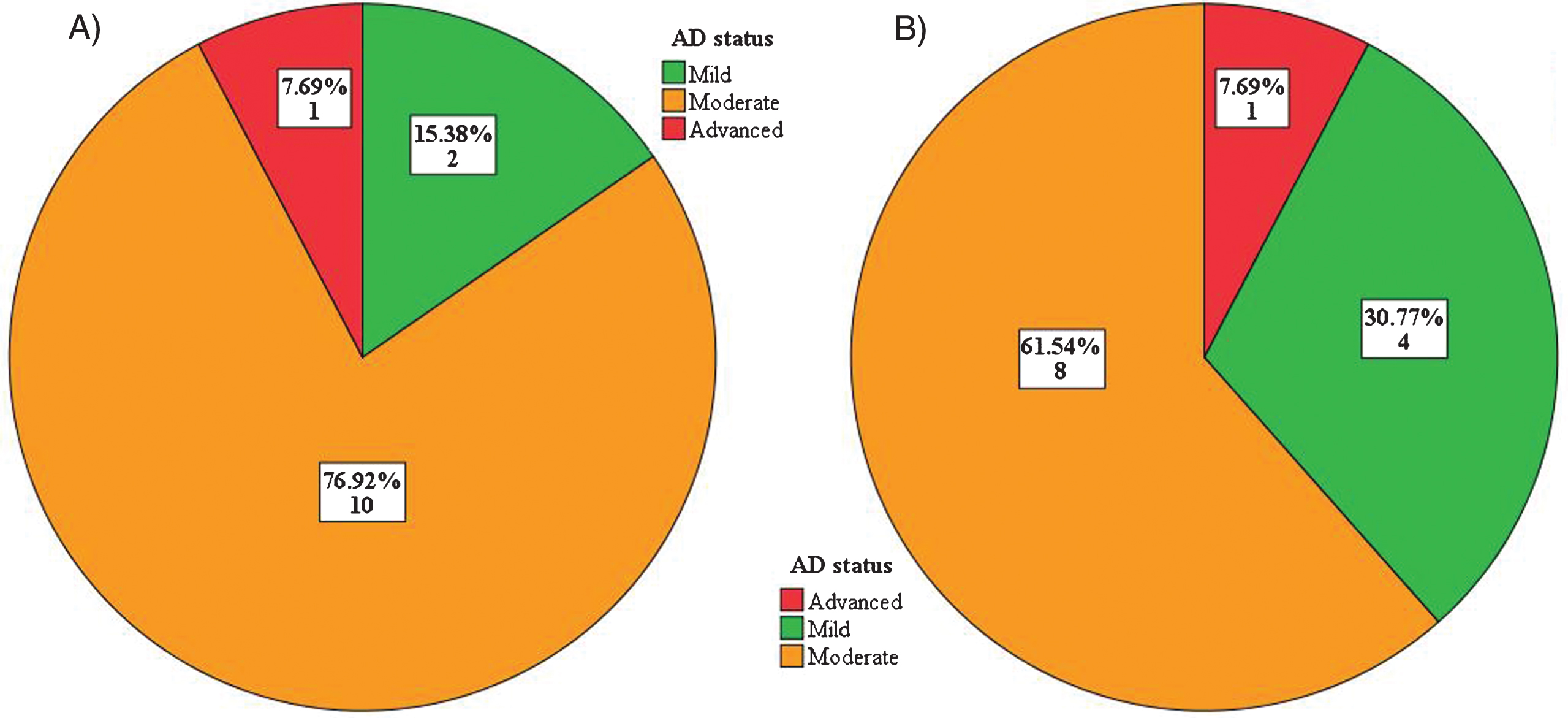
Table 2
Biochemical/clinical/functional response in patients with Alzheimer’s disease
| Study | Subject ID | Age (y) | Sex | Baseline MMSE score | Baseline AD Status | Baseline Serum L (μmol/L) | 6-months Serum L (μmol/L) | Baseline Serum Z (μmol/L) | 6-months Serum Z (μmol/L) | 6-months Serum MZ (μmol/L) | Observations at 18 months |
| Trial 1 | ADCD2 | 78 | M | 16 | Moderate | 0.072 | 0.666 | 0.006 | 0.062 | 0.08 | No difference reported |
| ADCD3 | 81 | M | 17 | Moderate | 0.432 | 0.933 | 0.046 | 0.088 | 0.044 | No difference reported | |
| ADCD4 | 84 | M | 18 | Moderate | 0.302 | 0.973 | 0.057 | 0.099 | 0.052 | No difference reported | |
| ADCD5 | 82 | F | 23 | Mild | 0.466 | 0.676 | 0.133 | 0.099 | 0.034 | No difference reported | |
| ADCD8 | 90 | F | 15 | Moderate | 0.149 | 0.564 | 0.032 | 0.056 | 0.043 | Patient too sick to continue in study | |
| ADCD9 | 76 | M | 22 | Mild | 0.325 | 1.631 | 0.076 | 0.189 | 0.086 | Patient in a nursing home | |
| ADCD11 | 68 | F | 19 | Moderate | 0.397 | 0.941 | 0.057 | 0.076 | 0.044 | No information available | |
| ADN24 | 68 | M | 23 | Mild | 0.149 | 0.285 | 0.054 | 0.041 | 0.014 | No difference reported | |
| ADN25 | 64 | F | 15 | Moderate | 0.202 | 0.771 | 0.035 | 0.078 | 0.027 | Patient unable to continue in study | |
| ADN26 | 74 | F | 21 | Mild | 0.364 | 1.972 | 0.059 | 0.248 | 0.294 | Patient unable to follow instruction | |
| ADN29 | 87 | F | 19 | Moderate | 0.238 | 2.415 | 0.02 | 0.245 | 0.234 | Patient too sick to continue in study | |
| ADN31 | 90 | M | 20 | Moderate | 0.034 | 0.364 | 0.003 | 0.024 | 0.018 | No difference reported | |
| Trial 2 | C3A4 | 79 | F | 12 | Moderate | 0.051 | 0.548 | 0.027 | 0.057 | 0.062 | Good improvement in memory |
| C3A5 | 78 | M | 22 | Mild | 0.204 | 1.733 | 0.05 | 0.145 | 0.1 | Good improvement in memory and sight | |
| C3A6 | 89 | F | 14 | Moderate | 0.273 | 3.599 | 0.089 | 0.312 | 0.228 | Subject was improved and manageable | |
| C3A7 | 81 | F | 13 | Moderate | 0.095 | 2.515 | 0.041 | 0.226 | 0.153 | No difference reported | |
| C3A8 | 87 | M | 17 | Moderate | 0.153 | 1.021 | 0.058 | 0.094 | 0.091 | No difference reported | |
| C3A9 | 88 | F | 21 | Mild | 0.122 | 0.536 | 0.069 | 0.082 | 0.03 | No difference reported | |
| C3A10 | 71 | F | 18 | Moderate | 0.107 | 2.722 | 0.026 | 0.244 | 0.186 | No difference reported | |
| C3A12 | 79 | F | 17 | Moderate | 0.244 | 2.229 | 0.075 | 0.153 | 0.152 | Good improvement in function | |
| C3A13 | 77 | M | 10 | Severe | 0.064 | 1.971 | 0.044 | 0.131 | 0.178 | No difference reported | |
| C3A14 | 69 | M | 17 | Moderate | 0.074 | 0.342 | 0.048 | 0.039 | 0.1 | No difference reported | |
| C3A16 | 87 | M | 18 | Moderate | 0.123 | 0.974 | 0.043 | 0.058 | 0.085 | Good improvement in memory | |
| C3A17 | 74 | F | 18 | Moderate | 0.315 | 1.879 | 0.137 | 0.065 | 0.252 | No difference reported | |
| C3A19 | 65 | F | 18 | Moderate | 0.182 | 1.97 | 0.105 | 0.148 | 0.226 | Good improvement in function |
Trial 1, patients with AD supplemented with Formulation 1; Formulation 1, 10 mg lutein, 10 mg meso-zeaxanthin, and 2 mg of zeaxanthin (carotenoid only); Trial 2, patients with AD supplemented with Formulation 2; Formulation 2, 10 mg lutein, 10 mg meso-zeaxanthin, and 2 mg of zeaxanthin plus 1 gram of fish oil (430 mg docohexaenoic acid [DHA] and 90 mg eicopentaenoic acid [EPA]) (carotenoid plus fish oil); methods); Serum L and Z, serum concentration of lutein and zeaxanthin measured in μmol/L; MMSE, Mini-Mental State Examination; Observations at 18-months, data at 18-months represents clinical and carer observations of patient health status and changes in health status.
However, as seen in Fig. 4A and 4B (data from Trial 2, xanthophyll carotenoid and fish oil intervention) and Table 2, progression of AD appeared much less, with carers reporting functional benefits in memory, sight, and mood. Pearson Chi-Square analysis demonstrated statistically significant between-group difference for the changes seen in AD status from baseline to 18-months (p = 0.003).
DISCUSSION
From this study, we propose that a combination of xanthophyll carotenoids and omega-3 fatty acids work synergistically to maintain function and quality of life in patients with AD. The findings from this work were unexpected, as the trials were not conducted to assess the impact of nutritional supplements on AD progression; rather, these trials were designed to measure biochemical response to xanthophyll carotenoid and omega-3 fatty acid supplementation [40, 41]. However, assessment of the patients (compiled from the research nurse reports, which included reports from the patient carers) presented very striking differences with regard to the health of the patients during the trial. Of importance, these differences were directly linked to the intervention group, where the positive outcomes were identified in patients consuming the combination of xanthophyll carotenoids and fish oil. Of note, this is the first scientific investigation reporting on the impact of a xanthophyll carotenoid and omega-3 intervention in patients with AD. Here, we examine the scientific rationale in support of our findings, and we do so below by discussing the role of nutrition in the brain under the following headings: AD pathogenesis; presence of xanthophyll carotenoids and omega-3 fatty acids in the brain; mechanisms of action; synergistic effect of nutrition.
There is currently no known cure for AD. Current management of AD involves drugs which aim to slow disease progression and improve cognition and behavior. Of note, only two drugs are in widespread clinical use. These include cholinesterase inhibitors and NMDA-receptor antagonists (memantine) [45, 46]. However, these drugs are associated with numerous adverse effects including gastrointestinal disturbance, rhinorrhoea, confusion and sedation. Cholinesterase inhibitor therapy is associated with a doubling of risk of hospitalization for bradycardia [47]. Also, cholinesterase inhibitors and memantine exert only a modest and temporary beneficial effect on cognitive function, mood, and behavior [45]. The existing pharmacological approach for the management of established AD remains unsatisfactory, thereby prompting increasing attention being directed toward preventative strategies for this condition [48]. Well-recognized modifiable risk factors for AD include smoking, diabetes, ischemic heart disease, hypertension, obesity, and dyslipidemia [49]. Also, there is a growing body of evidence that good nutrition is important for optimal cognition [50], maintenance of cognition [51], and is also associated with reduced risk of AD [7, 52].
Oxidative stress is believed to play a major role in the development of AD, and represents one of the earliest events of this condition [53]. The brain is particularly susceptible to oxidative damage because of the high oxygen demand and high proportion of polyunsaturated fatty acids in this neural tissue. In particular, the oxidation-reduction reactions necessary for the generation of Adenosine triphosphate (ATP) produce reactive oxygen species (ROS) as electrons are transferred from one molecule to another [54]. The generation of ROS (or free radicals) and associated cellular damage contributes to the pathology seen in susceptible neurons in AD. It is for this reason that antioxidants offer real potential for preventing AD.
As noted previously, the xanthophyll carotenoids L, Z, and MZ are found in their highest concentration at the macula (retina), which is part of the central nervous system. To date, L and Z have been identified in the hippocampus, cerebellum and frontal, occipital and temporal cortices [32, 33], and in amounts that correlate positively and significantly with their respective retinal concentrations [55]. Therefore, the retinal concentrations of these xanthophyll carotenoids (known as MP) can be used as a biomarker for these carotenoids in the brain. Interestingly, MP is positively related to cognitive performance in cognitively healthy individuals [56] and cognitively impaired individuals [57]. Indeed, data from our group has shown that xanthophyll carotenoid intervention (with a formulation containing L, MZ and Z; 10:10:2) in cognitively healthy individuals results in improvements in memory and function [39]. In another paper, we have shown that patients with AD have significantly lower serum xanthophyll carotenoid concentrations and MP levels compared to controls [41]. However, data on the impact of xanthophyll carotenoid intervention for patients with AD is limited. The emerging view that these xanthophyll carotenoids are neuro-protective is premised upon their chemical composition (i.e., amount of conjugated double-bonds and the presence of polar hydroxyl groups) and their localization within the lipid bi-layer of the cell membrane, thus bestowing antioxidant and anti-inflammatory activity at loci where they are needed [58, 59]. It has also been suggested that these xanthophyll carotenoids can enhance the structural integrity of membranes [60] and positively impact neural efficiency [61, 62].
Omega-3 fatty acids (especially DHA) are present in high concentrations in the human brain, but most of the studies to date have been conducted on the impact of fatty acids on brain development in infants [63]. DHA participates in a number of important neuronal processes including enhancement of membrane integrity and fluidity, neurogenesis, neuroplasticity, neuron differentiation and survival. Of interest, over the past 150 years, the Western diet has changed such that the ratio of omega-3 to omega-6 fatty acids has altered from 1:1 to 1:20, signifying that the Western diet is now deficient in omega-3 fatty acids [64]. This recent nutrient deficiency of DHA has most likely contributed to the increased prevalence and incidence AD, given the above outlined functions of DHA for the brain.
The results from the current study suggest that the improvements we identified in patients with AD were uniquely achieved only when a combination of the xanthophyll carotenoids and omega-3 fatty acids were provided to the patients. In this work, we observed noticeable differences between patients supplemented with xanthophyll carotenoids plus omega-3 fatty acids compared to patients supplemented with the xanthophyll carotenoids only, in terms of their health and function. In Trial 2, the “clinical story” for the patients was more positive than patients in Trial 1. In fact, the carers for patients in Trial 2 reported functional benefits in memory, sight and mood. Following completion of the trial, families and carers of the patients in Trial 2 have contacted our research center requesting continued access to the supplement, as they are adamant that the intervention with xanthophyll carotenoids and fish oil has had a very positive impact for the patient. We acknowledge that these reports are anecdotal. Also, our data demonstrates a superior biochemical (blood) response to the xanthophyll carotenoids when supplemented in combination with the omega-3 fatty acid (fish oil) compared to providing the exact same formulation of xanthophyll carotenoids (MZ:L:Z: 10:10:2) in the absence of fish oil. The improved delivery of these important brain nutrients to the target (neural) tissue is likely to have contributed to the positive outcomes linked to this formulation (i.e. via enhanced absorption and distribution of the carotenoids). Of note, this finding is consistent with a previous report by Johnson et al who showed that supplementation with DHA and lutein improve serum and MP levels in healthy elderly female subjects [65]. This finding may be explained by the hydrophobic nature of the xanthophyll carotenoids, as it is known that consuming carotenoid-rich foods in the presence of oils or cholesterol will increase carotenoid uptake and bio-accessibility [66].
It is important to point out that while the results of this study are very promising and offer hope for the management of AD, there are several limitations that need to be acknowledged. Firstly, the number of subjects in each Trial for this report was small and therefore our findings must only be viewed as preliminary. The findings presented here will need to be confirmed by a larger powered sample, and with appropriately definite outcome measures and study design. In the current trials, MMSE was only performed at baseline and we did not have the opportunity to capture specific outcome measures of functional or cognitive abilities. We acknowledge that such investigation is merited and will greatly aid our understanding of the positive outcomes reported here. Also, MP was not measured in Trial 2 patients, which represents another limitation of the current study.
In conclusion, this preliminary report, which is supported by a biologically plausible scientific rationale, suggests positive outcomes for patients with AD who consumed a combination of xanthophyll carotenoids and fish oil over an 18-month period. These patients demonstrated maintenance of cognitive and visual function that was not achieved when a xanthophyll carotenoid only intervention was used. We believe that the results of this study should guide a focused nutritional interventional strategy for patients with AD, but we acknowledge that these positive findings will need to be tested and confirmed with further study.
CONFLICT OF INTEREST
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/18-0160r2).
ACKNOWLEDGMENTS
CARDS was funded by the Howard Foundation (Registered UK Charity No: 285822). We thank the study participants and their carers for their participation and commitment to the project. We also acknowledge the senior research nurse manager (Maggie Bolger) and research technician (Ekaterina Loskutova) for their work on this project. We would also like to thank Professor Elizabeth Johnson from Tuffs University, USA, for permission to use the dietary L/Z screener for estimating dietary intake of lutein and zeaxanthin in this study and Albert Koulman and Larissa Richardson from the Medical Research Council Human Nutrition Research, Cambridge, UK for supporting lipid analysis. We are grateful for the advice from Professor David Thurnham (Northern Ireland Centre for Food and Health, [NICHE], University of Ulster Coleraine UK) during the preparation of our manuscript. We also wish to thank EPAX for providing the omega-3 fatty acids and Industrial Orgánica for providing the xanthophyll carotenoids used in this trial.
REFERENCES
[1] | Thakur KT , Albanese E , Giannakopoulos P , Jette N , Linde M , Prince MJ , Steiner TJ , Dua T ((2016) ) Neurological disorders. In Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4), Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora ME, eds. The International Bank for Reconstruction and Development / The World Bank (c) 2016 International Bank for Reconstruction and Development / The World Bank., Washington (DC). |
[2] | Wimo A , Guerchet M , Ali GC , Wu YT , Prina AM , Winblad B , Jonsson L , Liu Z , Prince M ((2017) ) The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement 13: , 1–7. |
[3] | Wimo A , Jonsson L , Bond J , Prince M , Winblad B ((2013) ) The worldwide economic impact of dementia 2010. Alzheimers Dement 9: , 1-11.e13. |
[4] | Wimo A , von Strauss E , Nordberg G , Sassi F , Johansson L ((2002) ) Time spent on informal and formal care giving for persons with dementia in Sweden. Health Policy 61: , 255–268. |
[5] | Alzheimer’s Association ((2017) ) 2017 Alzheimer’s disease facts and figures, Alzheimer’s Association, Chicago, IL, USA. |
[6] | Livingston G , Sommerlad A , Orgeta V , Costafreda SG , Huntley J , Ames D , Ballard C , Banerjee S , Burns A , Cohen-Mansfield J , Cooper C , Fox N , Gitlin LN , Howard R , Kales HC , Larson EB , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbaek G , Teri L , Mukadam N ((2017) ) Dementia prevention, intervention, and care. Lancet 390: , 2673–2734. |
[7] | Solfrizzi V , Custodero C , Lozupone M , Imbimbo BP , Valiani V , Agosti P , Schilardi A , D’Introno A , La Montagna M , Calvani M , Guerra V , Sardone R , Abbrescia DI , Bellomo A , Greco A , Daniele A , Seripa D , Logroscino G , Sabba C , Panza F ((2017) ) Relationships of dietary patterns, foods, and micro- and macronutrients with Alzheimer’s disease and late-life cognitive disorders: A systematic review. J Alzheimers Dis 59: , 815–849. |
[8] | Ozawa M, Ninomiya T, Ohara T, Doi Y, Uchida K, Shirota T, Yonemoto K, Kitazono T, Kiyohara Y ((2013) ) Dietary patterns and risk of dementia in an elderly Japanese population: The Hisayama Study. Am J Clin Nutr 97: , 1076–1082. |
[9] | Scarmeas N , Stern Y , Tang MX , Mayeux R , Luchsinger JA ((2006) ) Mediterranean diet and risk for Alzheimer’s disease. Ann Neurol 59: , 912–921. |
[10] | Tangney CC , Kwasny MJ , Li H , Wilson RS , Evans DA , Morris MC ((2011) ) Adherence to a Mediterranean-type dietary pattern and cognitive decline in a community population. Am J Clin Nutr 93: , 601–607. |
[11] | Feart C , Samieri C , Rondeau V , Amieva H , Portet F , Dartigues JF , Scarmeas N , Barberger-Gateau P ((2009) ) Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA 302: , 638–648. |
[12] | Trichopoulou A , Kyrozis A , Rossi M , Katsoulis M , Trichopoulos D , La Vecchia C , Lagiou P ((2015) ) Mediterranean diet and cognitive decline over time in an elderly Mediterranean population. Eur J Nutr 54: , 1311–1321. |
[13] | McEvoy CT , Guyer H , Langa KM , Yaffe K ((2017) ) Neuroprotective diets are associated with better cognitive function: The Health and Retirement Study. J Am Geriatr Soc 65: , 1857–1862. |
[14] | Lourida I , Soni M , Thompson-Coon J , Purandare N , Lang IA , Ukoumunne OC , Llewellyn DJ ((2013) ) Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology 24: , 479–489. |
[15] | Psaltopoulou T , Sergentanis TN , Panagiotakos DB , Sergentanis IN , Kosti R , Scarmeas N ((2013) ) Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann Neurol 74: , 580–591. |
[16] | Singh B , Parsaik AK , Mielke MM , Erwin PJ , Knopman DS , Petersen RC , Roberts RO ((2014) ) Association of Mediterranean diet with mild cognitive impairment and Alzheimer’s disease: A systematic review and meta-analysis. J Alzheimers Dis 39: , 271–282. |
[17] | Scarmeas N , Stern Y , Mayeux R , Manly JJ , Schupf N , Luchsinger JA ((2009) ) Mediterranean diet and mild cognitive impairment. Arch Neurol 66: , 216–225. |
[18] | Sofi F , Macchi C , Abbate R , Gensini GF , Casini A ((2014) ) Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17: , 2769–2782. |
[19] | Muldoon MF , Ryan CM , Yao JK , Conklin SM , Manuck SB ((2014) ) Long-chain omega-3 fatty acids and optimization of cognitive performance. Mil Med 179: , 95–105. |
[20] | Cole GM , Lim GP , Yang F , Teter B , Begum A , Ma Q , Harris-White ME , Frautschy SA ((2005) ) Prevention of Alzheimer’s disease: Omega-3 fatty acid and phenolic anti-oxidant interventions. Neurobiol Aging 26: (Suppl 1), 133–136. |
[21] | Fotuhi M , Mohassel P , Yaffe K ((2009) ) Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or Alzheimer disease: A complex association. Nat Clin Pract Neurol 5: , 140–152. |
[22] | Thomas J , Thomas CJ , Radcliffe J , Itsiopoulos C ((2015) ) Omega-3 fatty acids in early prevention of inflammatory neurodegenerative disease: A focus on Alzheimer’s disease. Biomed Res Int 2015: , 172801. |
[23] | Cole GM , Frautschy SA ((2010) ) DHA may prevent age-related dementia. J Nutr 140: , 869–874. |
[24] | Ammann EM , Pottala JV , Robinson JG , Espeland MA , Harris WS ((2017) ) Erythrocyte omega-3 fatty acids are inversely associated with incident dementia: Secondary analyses of longitudinal data from the Women’s Health Initiative Memory Study (WHIMS). Prostaglandins Leukot Essent Fatty Acids 121: , 68–75. |
[25] | Abubakari AR , Naderali MM , Naderali EK ((2014) ) Omega-3 fatty acid supplementation and cognitive function: Are smaller dosages more beneficial?. Int J Gen Med 7: , 463–473. |
[26] | Yurko-Mauro K , McCarthy D , Rom D , Nelson EB , Ryan AS , Blackwell A , Salem N Jr , Stedman M ((2010) ) Beneficial effects of docosahexaenoic acid on cognition in age-related cognitive decline. Alzheimers Dement 6: , 456–464. |
[27] | Phillips MA , Childs CE , Calder PC , Rogers PJ ((2015) ) No effect of omega-3 fatty acid supplementation on cognition and mood in individuals with cognitive impairment and probable Alzheimer’s disease: A randomised controlled trial. Int J Mol Sci 16: , 24600–24613. |
[28] | van de Rest O , Geleijnse JM , Kok FJ , van Staveren WA , Dullemeijer C , Olderikkert MG , Beekman AT , de Groot CP ((2008) ) Effect of fish oil on cognitive performance in older subjects: A randomized, controlled trial. Neurology 71: , 430–438. |
[29] | Perry A , Rasmussen H , Johnson EJ ((2009) ) Xanthophyll (lutein, zeaxanthin) content in fruits, vegetables and corn and egg products. J Food Compost Anal 22: , 9–15. |
[30] | Prado-Cabrero A , Beatty S , Stack J , Howard A , Nolan JM ((2016) ) Quantification of zeaxanthin stereoisomers and lutein in trout flesh using chiral high-performance liquid chromatography-diode array detection. J Food Compost Anal 50: , 19–22. |
[31] | Neuringer M , Sandstrom MM , Johnson EJ , Snodderly DM ((2004) ) Nutritional manipulation of primate retinas, I: Effects of lutein or zeaxanthin supplements on serum and macular pigment in xanthophyll-free rhesus monkeys. Invest Ophthalmol Vis Sci 45: , 3234–3243. |
[32] | Johnson EJ , Vishwanathan R , Johnson MA , Hausman DB , Davey A , Scott TM , Green RC , Miller LS , Gearing M , Woodard J , Nelson PT , Chung HY , Schalch W , Wittwer J , Poon LW ((2013) ) Relationship between serum and brain carotenoids, alpha-tocopherol, and retinol concentrations and cognitive performance in the oldest old from the Georgia Centenarian Study. J Aging Res 2013: , 951786. |
[33] | Craft NE , Haitema TB , Garnett KM , Fitch KA , Dorey CK ((2004) ) Carotenoid, tocopherol, and retinol concentrations in elderly human brain. J Nutr Health Aging 8: , 156–162. |
[34] | Feart C , Letenneur L , Helmer C , Samieri C , Schalch W , Etheve S , Delcourt C , Dartigues JF , Barberger-Gateau P ((2016) ) Plasma carotenoids are inversely associated with dementia risk in an elderly French cohort. J Gerontol A Biol Sci Med Sci 71: , 683–688. |
[35] | Min JY , Min KB ((2014) ) Serum lycopene, lutein and zeaxanthin, and the risk of Alzheimer’s disease mortality in older adults. Dement Geriatr Cogn Disord 37: , 246–256. |
[36] | Loef M , Walach H ((2012) ) Fruit, vegetables and prevention of cognitive decline or dementia: A systematic review of cohort studies. J Nutr Health Aging 16: , 626–630. |
[37] | Hammond BR Jr , Miller LS , Bello MO , Lindbergh CA , Mewborn C , Renzi-Hammond LM ((2017) ) Effects of lutein/zeaxanthin supplementation on the cognitive function of community dwelling older adults: A randomized, double-masked, placebo-controlled trial. Front Aging Neurosci 9: , 254. |
[38] | Johnson EJ , McDonald K , Caldarella SM , Chung HY , Troen AM , Snodderly DM ((2008) ) Cognitive findings of an exploratory trial of docosahexaenoic acid and lutein supplementation in older women. Nutr Neurosci 11: , 75–83. |
[39] | Power R , Coen RF , Beatty S , Mulcahy R , Moran R , Stack J , Howard AN , Nolan JM ((2018) ) Supplemental retinal carotenoids enhance memory in healthy individuals with low levels of macular pigment in a randomized, double-blind, placebo-controlled clinical trial. J Alzheimers Dis 61: , 947–961. |
[40] | Nolan JM , Loskutova E , Howard A , Mulcahy R , Moran R , Stack J , Bolger M , Coen RF , Dennison J , Akuffo KO , Owens N , Power R , Thurnham D , Beatty S ((2015) ) The impact of supplemental macular carotenoids in Alzheimer’s disease: A randomized clinical trial. J Alzheimers Dis 44: , 1157–1169. |
[41] | Nolan JM , Loskutova E , Howard AN , Moran R , Mulcahy R , Stack J , Bolger M , Dennison J , Akuffo KO , Owens N , Thurnham DI , Beatty S ((2014) ) Macular Pigment, visual function, and macular disease among subjects with Alzheimer’s disease: An exploratory study. J Alzheimers Dis 42: , 1191–1202. |
[42] | Thurnham DI , Tremel A , Howard AN ((2008) ) A supplementation study in human subjects with a combination of meso-zeaxanthin, (3R,3’R)-zeaxanthin and (3R,3’R,6’R)-lutein. Br J Nutr 100: , 1307–1314. |
[43] | Lu L , Koulman A , Petry CJ , Jenkins B , Matthews L , Hughes IA , Acerini CL , Ong KK , Dunger DB ((2016) ) An unbiased lipidomics approach identifies early second trimester lipids predictive of maternal glycemic traits and gestational diabetes mellitus. Diabetes Care 39: , 2232–2239. |
[44] | Akuffo KO , Beatty S , Stack J , Peto T , Leung I , Corcoran L , Power R , Nolan JM ((2015) ) Concordance of macular pigment measurement using customized heterochromatic flicker photometry and fundus autofluorescence in age-related macular degeneration. Invest Ophthalmol Vis Sci 56: , 8207–8214. |
[45] | Blennow K , de Leon MJ , Zetterberg H ((2006) ) Alzheimer’s disease. Lancet 368: , 387–403. |
[46] | Bullock R , Touchon J , Bergman H , Gambina G , He Y , Rapatz G , Nagel J , Lane R ((2005) ) Rivastigmine and donepezil treatment in moderate to moderately-severe Alzheimer’s disease over a 2-year period. Curr Med Res Opin 21: , 1317–1327. |
[47] | Park-Wyllie LY , Mamdani MM , Li P , Gill SS , Laupacis A , Juurlink DN ((2009) ) Cholinesterase inhibitors and hospitalization for bradycardia: A population-based study. PLoS Med 6: , e1000157. |
[48] | French Pharmacoeconomic Committee ((2012) ) Drugs for Alzheimer’s disease: Best avoided. No therapeutic advantage. Prescrire Int 21: , 150. |
[49] | Qiu C ((2012) ) Preventing Alzheimer’s disease by targeting vascular risk factors: Hope and gap. J Alzheimers Dis 32: , 721–731. |
[50] | Valls-Pedret C , Sala-Vila A , Serra-Mir M , Corella D , de la Torre R , Martinez-Gonzalez MA , Martinez-Lapiscina EH , Fito M , Perez-Heras A , Salas-Salvado J , Estruch R , Ros E ((2015) ) Mediterranean diet and age-related cognitive decline: A randomized clinical trial. JAMA Intern Med 175: , 1094–1103. |
[51] | Pelletier A , Barul C , Feart C , Helmer C , Bernard C , Periot O , Dilharreguy B , Dartigues JF , Allard M , Barberger-Gateau P , Catheline G , Samieri C ((2015) ) Mediterranean diet and preserved brain structural connectivity in older subjects. Alzheimers Dement 11: , 1023–1031. |
[52] | Otaegui-Arrazola A , Amiano P , Elbusto A , Urdaneta E , Martinez-Lage P ((2014) ) Diet, cognition, and Alzheimer’s disease: Food for thought. Eur J Nutr 53: , 1–23. |
[53] | Zhu X , Su B , Wang X , Smith MA , Perry G ((2007) ) Causes of oxidative stress in Alzheimer disease. Cell Mol Life Sci 64: , 2202–2210. |
[54] | Bonda DJ , Wang X , Perry G , Nunomura A , Tabaton M , Zhu X , Smith MA ((2010) ) Oxidative stress in Alzheimer disease: A possibility for prevention. Neuropharmacology 59: , 290–294. |
[55] | Vishwanathan R , Schalch W , Johnson EJ ((2016) ) Macular pigment carotenoids in the retina and occipital cortex are related in humans. Nutr Neurosci 19: , 95–101. |
[56] | Feeney J , Finucane C , Savva GM , Cronin H , Beatty S , Nolan JM , Kenny RA ((2013) ) Low macular pigment optical density is associated with lower cognitive performance in a large, population-based sample of older adults. Neurobiol Aging 34: , 2449–2456. |
[57] | Renzi LM , Dengler MJ , Puente A , Miller LS , Hammond BR Jr ((2014) ) Relationships between macular pigment optical density and cognitive function in unimpaired and mildly cognitively impaired older adults. Neurobiol Aging 35: , 1695–1699. |
[58] | Landrum JT , Bone RA ((2001) ) Lutein, zeaxanthin, and the macular pigment. Arch Biochem Biophys 385: , 28–40. |
[59] | Bian Q , Gao S , Zhou J , Qin J , Taylor A , Johnson EJ , Tang G , Sparrow JR , Gierhart D , Shang F ((2012) ) Lutein and zeaxanthin supplementation reduces photooxidative damage and modulates the expression of inflammation-related genes in retinal pigment epithelial cells. Free Radic Biol Med 53: , 1298–1307. |
[60] | Zamroziewicz MK , Paul EJ , Zwilling CE , Johnson EJ , Kuchan MJ , Cohen NJ , Barbey AK ((2016) ) Parahippocampal cortex mediates the relationship between lutein and crystallized intelligence in healthy, older adults. Front Aging Neurosci 8: , 297. |
[61] | Bovier ER , Hammond BR ((2015) ) A randomized placebo-controlled study on the effects of lutein and zeaxanthin on visual processing speed in young healthy subjects. Arch. Biochem. Biophys 572: , 54–57. |
[62] | Lindbergh CA , Mewborn CM , Hammond BR , Renzi-Hammond LM , Curran-Celentano JM , Miller LS ((2017) ) Relationship of lutein and zeaxanthin levels to neurocognitive functioning: An fMRI study of older adults. J Int Neuropsychol Soc 23: , 11–22. |
[63] | Parletta N , Milte CM , Meyer BJ ((2013) ) Nutritional modulation of cognitive function and mental health. J Nutr Biochem 24: , 725–743. |
[64] | Simopoulos AP ((2011) ) Evolutionary aspects of diet: The omega-6/omega-3 ratio and the brain. Mol Neurobiol 44: , 203–215. |
[65] | Johnson EJ , Chung HY , Caldarella SM , Snodderly DM ((2008) ) The influence of supplemental lutein and docosahexaenoic acid on serum, lipoproteins, and macular pigmentation. Am J Clin Nutr 87: , 1521–1529. |
[66] | van Het Hof KH , West CE , Weststrate JA , Hautvast JG ((2000) ) Dietary factors that affect the bioavailability of carotenoids. J Nutr 130: , 503–506. |



